The Bland-White-Garland syndrome – the anomalous origin of the left coronary artery (LCA) from the pulmonary artery (PA) – is a very rare congenital abnormality affecting 1 in 300,000 live births [1–3]. This defect is associated with extremely high mortality in infants, reaching nearly 90%; hence late presentation of the Bland-White-Garland syndrome is very unusual [1–3].
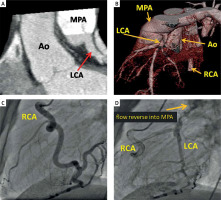
A 24-year-old woman was admitted to our center due to impaired exercise tolerance. The electrocardiogram showed signs of prior antero-lateral myocardial infarction (pathologic Q waves in leads V3-V6, I, aVL). Echocardiography demonstrated reduced left ventricular ejection fraction (LVEF = 38%) with akinesia of apical and medial segments of anterior and lateral walls. Coronary computed tomography angiography and coronary angiography showed the anomalous origin of the LCA from the pulmonary artery and the dominant right coronary artery supplying the LCA through very numerous, prominent collaterals (Figures 1 A–D). Additionally, reverse flow of a contrast agent from the LCA into the pulmonary artery was observed (Figure 1 D). On the basis of these two imaging examinations, the Bland-White-Garland syndrome was diagnosed.
Figure 1
The anomalous origin of the left coronary artery (LCA) from the pulmonary artery (MPA) on computed tomography scans (A, B) and coronary angiograms (C, D)
RCA – right coronary artery, Ao – aorta.
The coronary steal phenomenon and retrograde left-sided coronary flow may lead to subendocardial ischemia/necrosis with subsequent left ventricular dysfunction and increased risk of malignant ventricular arrhythmias and sudden cardiac death [1, 3]. Therefore, the patient was scheduled for surgical treatment – bypassing the left anterior descending artery (LAD) with the use of the left internal mammary artery (LIMA) and ligation of the anomalous LCA origin. The left circumflex artery was recessive and had a small luminal diameter; hence it was not bypassed. At discharge, the patient was administered a β-blocker, an angiotensin-converting enzyme inhibitor and an aldosterone antagonist. The patient did not experience any major adverse cardiac event during the 5-year follow-up period; however, the recovery of left ventricular systolic function was not complete and LVEF remained mildly reduced (LVEF = 45%).
Apart from the above-mentioned coronary artery bypass grafting, there are two alternative treatment options. The translocation procedure, used more frequently, involves direct re-implantation of the anomalously originated left coronary artery into the aorta. However, this technique is not suitable if the LCA origin is located far from the aorta. In such a situation, the Takeuchi procedure might be preferred. It involves creation of an aortopulmonary window and an intrapulmonary tunnel that baffles the aorta to the ostium of the anomalous left coronary artery [2, 4]. Regardless of the applied surgical technique, restoration of normal coronary flow limits the area of left ventricle ischemia/necrosis, reduces the risk of complex ventricular arrhythmias and improves the long-term prognosis [1, 2, 4, 5].
The Bland-White-Garland syndrome is a rare presentation in adulthood. However, once it is diagnosed, early surgical correction is recommended even in asymptomatic adult patients [1, 2, 4, 5].








