PURPOSE
Scleroderma is a multisystemic disorder characterised by inflammatory and vascular anomalies, and excess fibrosis. Progressive systemic sclerosis (PSS) mainly progresses with skin, joint, lung, heart, and kidney involvement. Localised scleroderma is characterised by skin involvement only [1, 2]. The incidence and prevalence of scleroderma can show significant differences in relation to ethnic and regional factors. Involvement of cerebral vessels is rare in both localised scleroderma and PSS. Transient ischemic attack and stroke are rare complications of scleroderma. Among other connective tissue diseases, systemic lupus erythematosus and polyarteritis nodosa can have neurological involvement [1-3].
Transient global amnesia (TGA) is a rare medical condition in which a person experiences a sudden episode of amnesia. During a TGA episode, the person is unable to form new memories (anterograde amnesia) and has difficulty recalling recent memories (retrograde amnesia). TGA usually takes no more than a few hours. In rare cases, it can take up to twenty-four hours. People with TGA remember who they are and can remember friends and family members. They can still perform complex daily tasks, such as cooking or driving a car. They also retain their language and social interaction skills. However, they may not know the day or the time, or where they are [4, 5].
In this report, an example of localised scleroderma and central nervous system involvement in a patient with ischemic stroke, who presented with speech disorder, occasional temporary memory loss, hearing loss, and inability to name objects, is presented.
CASE DESCRIPTION
A 60-year-old male patient presented to the emergency department of our hospital with speech impairment, forgetting words, occasional temporary memory loss, and hearing loss, which had started two days before.
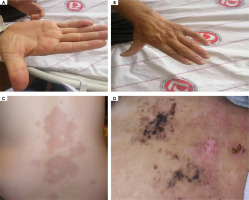
During physical examination of the patient at the time of admission, the following was recorded: temperature 36.7°C, blood pressure 140/100 mmHg, pulse 72/min, respiration 19/minute, oxygen saturation 97%, and electrocardiography was in normal sinus rhythm. During neurological examination, he was conscious, cooperative, and oriented; his pupils were isochoric, light reflex and corneal reflex were bilaterally normal. Eye movements were free in all directions. There was no paresis in the motor system examination of the extremities. His reflexes were normoactive in his lower and upper extremities, and the plantar response was flexor in both lower extremities. The patient had remembering new information or recalling the names of objects from the long-term memory. According to the information received from his relatives, he was experiencing occasional memory loss. There was thinning of the skin in the whole body, especially in the distal extremities and on the face. Flexion contracture was present in the proximal interphalangeal joints of the right hand and the skin was tight. He had a lesion on his back that was itchy for ten months a year, and itching went away for two months (Figure 1).
Figure 1
Flexion contracture was present in the right hand proximal interphalangeal joints and the skin was tight. He has an itchy lesion on his back
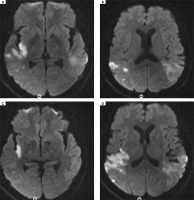
No evident acute pathology was detected in the brain computed tomography (CT) taken in the emergency department. In the brain magnetic resonance imaging (MRI) taken in the emergency room, diffusion restriction suggesting acute infarction in the right temporoparietal junction and findings suggesting acute-subacute infarction in the left parietotemporal junction were observed (Figure 2).
Figure 2
Acute and subacute infarction in the right temporoparietal junction and left parietotemporal junction
The patient, who had no known disease, medication, trauma, or history of febrile illness, was admitted to the neurology service with a preliminary diagnosis of ischemic stroke and due to further examination and treatment. The modified Rankin Scale (mRS) calculated at the first admission of the patient to the emergency department was evaluated as 2 and the NIH Stroke Scale/Score (NIHHS) was 4.
Routine blood tests, biochemistry, whole blood, lipid panel, B12 tests, thyroid function tests, HbA1c, erythrocyte sedimentation rate, serum electrophoresis, autoantibody screening (anti-SSA, anti-SSB), antithyroid antibodies, syphilis serology (fluorescent treponemal antibody), Schirmer test, prothrombin time, INR, PTT, homocysteine, anticardiolipin, rheumatoid factor, protein C and S, anti-streptolysin O, rheumatoid factor, and immunoglobin A, G, M were normal. Elisa tests (hepatitis A, HIV, hepatitis B, hepatitis C) were negative. Anti- nuclear antibody and anti-topoisomerase I (scl-70) positivity were detected. Complete urinalysis was within normal limits. When viral meningitis agents (herpes simplex virus 1-2, varicella zoster virus, enterovirus, parechovirus, Ebstein-Barr virus, cytomegalovirus, adenovirus) were investigated, and no agent was found. Brucella tests came back negative. The pathergy test for Behçet was negative.
Lumbar puncture results – glucose, chloride, lactate dehydrogenase, protein, lactate measured in the cerebrospinal fluid (CSF) were within normal limits. Oligoclonal bands and neuromyelitis optica were negative. The limbic and paraneoplastic panel viewed from CSF was normal.
No significant stenosis was detected in the cranial neck CT angiography of the patient. No significant stenosis was detected in the carotid-vertebra Doppler ultrasound performed on the patient.
No cardioembolic source was detected in the echocardiogram performed for ischemic stroke. No pathological finding was detected in the 24-hour rhythm Holter examination. Left atrium diameter was 3.1 cm.
In the thorax CT, there was segmental-subsegmental moderate atelectasis in the right lung base and minimal pleural effusion in the right hemithorax. No pathology was detected in the abdominal ultrasound.
The presence of increased collagen in the skin biopsy of the patient suggested scleroderma.
The patient was treated with acetylsalicylic acid 300 mg per day from the day he was admitted to our clinic with the diagnosis of stroke. At discharge, mRS was calculated as 1 and NIHHS 2.
The patient, whose symptoms regressed, was discharged with neurology and dermatology controls. Since the patient did not come to follow-ups, new brain imaging could not be taken.
COMMENT
The patient was diagnosed with localised scleroderma because of skin findings, autoantibody positivity for scleroderma, and absence of visceral involvement.
Although TGA can occur in various disorders, pathophysiologically, it most frequently occurs secondary to cerebrovascular dysfunction. In our case, cerebrovascular dysfunction was also dominant.
Scleroderma is a disease that progresses with increased collagen production due to increased activity of transforming growth factor beta (TGF-β) in almost every organ. It progresses with especially gastrointestinal system, lung, kidney, and skin involvement. It can also involve the central nervous system and reveal neurological findings [1, 6, 7].
The pathogenesis of PSS is not fully understood, but vascular or dysimmune mechanisms have been hypothesised.
According to the vascular mechanism, arterial and arteriolar medial hypertrophy resulting in fibrinoid necrosis in the vessels, endothelial changes and microangiopathy in the vase nervosum afterwards, increase the tendency of platelet aggregation to cause tissue ischemia and cerebrovascular disease.
Depending on the dysimmune mechanism, autoantibody formation is in question. This mechanism is in question in inflammatory myositis characterised by perivascular T cell and macrophage infiltration.
With the changes in collagen metabolism, a fibrotic process develops in the perineurium and epineurium, resulting in mononeuropathy in the peripheral nerves [1, 2].
Central nervous system involvement is thought to be due to vasospasm caused by the disease, and thromboembolism may be seen due to an increased susceptibility to thrombosis due to this vasospasm. Stroke may occur due to occlusion of cerebral vessels, including different symptoms that may occur depending on the vascular irrigation area in the brain [1, 2, 6]. As seen in the series of 50 patients with scleroderma published in 1992, cerebrovascular disease was found in 6-7% of the patients, peripheral neuropathy – in 20%, myelopathy – in 8%, and muscle involvement – in 22%. Findings, such as amnesia, can be seen [1-3].
In the case we presented, no pathology was found in the clinical and laboratory tests performed in terms of ischemic risk factors. Skin findings were contracture, skin biopsy results and antibody positivity related to scleroderma were observed. Considering the current pathogenesis of scleroderma, the patient’s ischemic stroke was thought to be the cause or facilitating factor.







