Coronary artery fistulas (CAFs) are uncommon cardiac abnormalities that affect 0.1% to 0.2% of people. There is an anomalous connection of one or more coronary arteries to a heart chamber cavity or great vessel. A coronary artery fistula ending in a chamber of the heart is called a coronary-cameral fistula (CCF) or, if connected to any segment of the systemic or pulmonary circulation, is termed a coronary arteriovenous fistula (CAVF). The pathophysiologies of both these lesions are identical, and they are often collectively termed under CAF. Compared to acquired fistulas, congenital ones are more typical with different presentations [1].
At the early stages of embryogenesis, they develop as a result of the enduring sinusoid connections between the primordial tubular heart’s lumens. As a result of distal run-off from the coronary vasculature into the receiving cavity with low pressure especially to right-sided chambers, myocardial steal and chamber enlargement occur. The majority of coronary artery fistulae are minor and asymptomatic without any side effects. Nonetheless, large fistulae may result in pathophysiological consequences. Due to the rarity of symptomatic fistulas, there is no agreement on the best course of treatment. Conservative medical management with regular observation, trans-catheter interventional closure, and surgical repair is described [2].
A 23-year-old woman presented to us with complaints of recurrent exertional chest pain with shortness of breath over 6 months. She had dyspnea that started slowly and progressed from New York Heart Classification (NYHA) grade II to III during the previous 2 months. Clinical examination revealed a moderate build, with a heart rate of 88/min, regular, and low-volume, and a blood pressure of 118/72 mm Hg. On auscultation, a continuous murmur was heard over the precordial region and maximally audible along the right sternal border, with another diastolic murmur over the aortic region. The remainder of the physical examination was within normal limits. The results of the patient’s blood tests were normal. The electrocardiography (ECG) showed a myocardial ischemia pattern in the right coronary territory with features of right-sided chamber dilatation. The transthoracic two-dimensional echocardiography revealed a large tunnel originating from the ascending aorta and connected to the right atrium (RA) with a continuous left-to-right shunt, and a maximum gradient of 36 mm Hg. All four cardiac chambers, the main pulmonary artery, and the left and right pulmonary arteries were dilated. There was holo-diastolic flow reversal in the descending and abdominal aorta. The cardiac valves were normal, with no septal abnormality. There was no intracavitary clot or vegetation. The left ventricle ejection fraction was assessed to be 50%.
Multislice cardiac computed tomography (CT) angiography and later 3-dimensional reconstruction images revealed a significantly dilated, tortuous right coronary artery (RCA) with a dilated, lobulated, tortuous fistulous track (that measured 18.3 mm near the origin). A 32 mm-caliber dilated lobulated component in the right anterior atrioventricular groove was causing compression over the tricuspid valve. The interatrial septum’s fistulous course was noticeably dilated (49 mm), culminating in the RA through a major and multiple tiny openings, which are suggestive of an RCA to RA fistula (Figures 1, 2). Conventional coronary angiography confirmed these findings. Imaging results with the ongoing ischemic symptoms confirmed the diagnosis of right-sided CCF in this patient. After being stabilized, she was taken up for surgical repair of CCF. Intraoperative examination revealed that the RA and right atrial appendage were hugely dilated. The RCA followed a tortuous path over the right atrioventricular groove and opened into the RA. Standard surgical steps included aorto-bicaval cannulation, antegrade cardioplegia, and moderate hypothermia on cardiopulmonary bypass. The RA was opened after caval snugging. The distal arterial fistula opening was closed by an autologous pericardial patch inside the RA. The rest of the lobulated, dilated RCA was also closed (Figure 2). A reverse saphenous vein bypass graft (RSVG) was placed from the ascending aorta to the distal RCA. There were no notable postoperative issues. After surgery, her ischemic symptoms were reduced and she has been on regular monthly follow-ups with antiplatelet medications for the last 6 months.
Figure 1
Three-dimensional reconstruction of coronary CT angiography showing an enlarged, lobulated component of the right coronary artery (RCA) originating from the ascending aorta (Ao) with a tortuous tract of the dilated RCA and fistulous opening in the RA
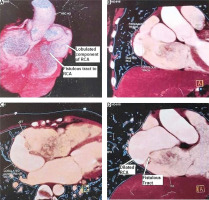
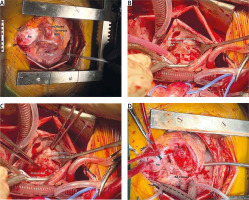
Figure 2
Intra-operative photographs: A – Dilated, tortuous right coronary artery (RCA) arising from the ascending aorta (Ao) and terminating in the right atrium (RA). B, C – Fistulous openings inside the RA; the major opening was closed with a pericardial patch from inside the RA. D – Proximal end of the RCA separated from the atrioventricular groove and lobulated portion closed
The majority of CAFs including CCFs have a congenital basis. They could develop as a result of a surgical procedure, an infection, or trauma. 0.08% to 0.3% of randomly chosen patients having diagnostic coronary angiography have been documented to have CCFs. Each fistula is identified and defined by the location of its origin and termination. The most common type of coronary artery fistula is one that arises from the RCA and empties into the right ventricle (RV). The RA or RV is where the majority of fistulae end, while the left atrium and left ventricle are uncommon distal opening places [3].
Most CCFs would be tiny and asymptomatic due to the unimpeded myocardial blood flow. However, with age, these little CCFs frequently become larger and can cause clinical symptoms in people who are not treated. The main pathophysiological explanation behind coronary fistula symptomatology is distal myocardial stealing [4]. As seen in our case, this large-size fistula had diastolic runoff, which results in coronary steal with a left-to-right shunt, as the fistula empties into the systemic venous side. CT angiography or conventional coronary angiography is used to precisely diagnose and identify the source of the fistula and course with termination for the treatment plan. The decision for fistula management is variable and depends on several factors, including symptoms, type, size, distal opening site, length and team expertise. Small fistulae are often asymptomatic, and may even close gradually. Small CCFs in general can be monitored with echocardiographic or angiographic follow-up to detect the expansion of feeding vessels with time [5].
Closure is essential for large CCFs. Transcatheter embolization and surgical closure are the two available methods. If a trans-catheter intervention is planned, there should be a specific focus on imaging studies to find the exact anatomy to choose the correct and individualized method. Percutaneous trans-catheter interventional management is now the first line and is feasible in most patients, with excellent long-term outcomes. Trans-catheter closure by various devices, vascular plug, embolizing particles or coils has been successfully done in cases of CCF with a single drainage site, non-tortuous vessel, distal narrowing of the fistula with a convenient path for delivery of the closure device, absence of important branches, absence of other coexisting disorders or for high surgical risk cases [6]. However, the trans-catheter approach may be unsuitable in cases of extreme tortuosity, multiple drainage opening sites and important coronary branches at the site of device positioning. Moreover, individuals with large fistulae, aneurysmal dilatation, or acute angulations that are not suitable for trans-catheter closure may require surgical closure despite the risk of cardiopulmonary bypass. Also due to very small vessels in the pediatric patient, catheter intervention may not be the appropriate choice. The available options for surgical intervention are coronary artery bypass grafting (CABG), reimplantation, or unroofing (marsupialization) of the anomalous coronary vessel after distal closure. The choice of method also depends on the competence of the treating team [7].
In our case there was a dilated, tortuous right coronary artery with steal phenomenon due to runoff towards the low-pressure chamber with multiple openings. Considering these facts, open surgery was chosen as an appropriate intervention with a successful outcome.
CCFs are uncommon congenital cardiac abnormalities and are mostly asymptomatic. As symptomatic fistulae are rare, currently there is no established, standard treatment policy for the best management. In addition to conservative medical care, trans-catheter intervention and surgical closure are available options for these rare anomalies. The addition of this unusual case report with a successful surgical outcome will add knowledge to the available medical literature.






