Fish tank granuloma, typically stemming from skin trauma following contact with Mycobacterium marinum (M. marinum)-contaminated water or infected fish. It is estimated that the annual incidence varies from 0.04 to 0.27 per 100,000 persons in different countries [1]. A lack of suspicion frequently leads to delayed diagnosis. Here, we present the case of a male with a longstanding hobby of fishing, emphasizing the necessity of considering uncommon pathogens in the differential diagnosis of persistent cutaneous lesions.
A 37-year-old man presented with a painless plaque and nodules on his right thigh and hip that had been persisting for more than 2 years. Initially diagnosed as tinea cruris, he received oral and topical antifungal drugs without resolution. The patient did not have a history of tuberculosis or any other systemic illness. Physical examination revealed an irregular polycyclic hyperkeratotic plaque with crusts on the surface and central regression on the dorsal proximal right thigh, along with three red nodules on the right hip (Figure 1). Routine laboratory tests were within normal ranges.
Figure 1
A hyperkeratotic plaque on the dorsal proximal right thigh, along with three red nodules on the right hip

The histopathological analysis showed non-caseating granulomas of histiocytes in the dermis, encircled by neutrophils, multinucleated giant cells, lymphocytes and an increase in collagen fibre formation. The overlying epidermis is hyperkeratotic and acanthotic (Figure 2 A, B). Skin tissue smear presented positive acid-fast stain (Figure 2 C). Additional testing of bacteria, fungi and mycobacteria in tissue culture further confirmed the presence of infection by M. marinum, which is consistent with the result of polymerase chain reaction (PCR). These findings confirmed the diagnosis of fish tank granuloma. The patient commenced treatment with rifampin, ethambutol, clarithromycin, and moxifloxacin, leading to complete regression of all lesions after a 4-month course.
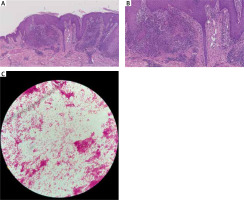
Figure 2
A, B – Histopathological findings revealed hyperkeratosis and acanthosis in epidermis and non-caseating granulomas of histiocytes in dermis. Haematoxylin and eosin stain, at original magnification (A) × 2.5 and (B) × 10. C – Skin tissue smear presented positive acid-fast stain
Given that the optimal temperature for M. marinum growth is 30 to 32°C, the infection mainly targets the skin. The clinical presentations are characterized by four patterns [2]: Type I presents as single erosive, or verrucous plaques as in this case. Type II exhibits numerous lesions in sporotrichoid distribution. Type III includes serious infections like tenosynovitis, arthritis and osteomyelitis. Type IV is characterized by disseminated lesions and systemic involvement, which is observed in immunocompromised patients or patients undergoing tumour necrosis factor (TNF) inhibitors therapy [3].
Histopathologic findings are contingent upon the lesion’s duration. During the early months, a non-specific inflammatory infiltrate may be detectable. The lesion then displays tuberculoid granulomas with fibrinoid masses as a defining feature. The epidermis shows signs of hyperkeratosis, acanthosis, pseudoepitheliomatous hyperplasia intraepidermal neutrophilic abscesses and ulceration [4]. M. marinum is difficult to find in immunocompetent individuals [2]. Culture is the standard method of identification and culture positivity rates fall within the 70% to 80% range. The PCR amplification technique proves to be a sensitive and specific diagnostic tool [5].
The average time from clinical presentation to correct diagnosis ranges from 1 to 27 months with a mean interval of 7 months [6], highlighting the diagnostic challenge posed by M. marinum infections. Lack of awareness and failure to obtain relevant medical history, such as aquatic exposure, contribute to this challenge.
Treatment for M. marinum infections is guided by the outcomes described in case reports. Initial treatment for localized forms typically includes monotherapy of the following antibiotics: clarithromycin, trimethoprim-sulfamethoxazole, minocycline or doxycycline [6, 7]. Combination therapy, often involving clarithromycin plus rifampin and/or ethambutol, is preferred for extensive infection or deep tissue involvement [8]. The treatment should be maintained for an additional 2 months following clinical recovery.
The upper limbs have been consistently afflicted [9]. In contrast, the involvement of lower extremities is infrequent, and it is typically limited to the knee and shin [6]. Involvement of the thigh and hip is uncommon. Therefore, we would like to highlight the importance of considering uncommon pathogens in cases of chronic cutaneous lesions in which previous treatments have failed, particularly in patients with relevant exposures or hobbies.








