Introduction
Menopause is a physiological transition in a woman’s life and is the result of decreased production of ovarian gonadotropins, oestrogen, and progesterone [1, 2]. Although some women go through the menopausal transition without symptoms, changes observed in a hormonal profile of women at midlife are directly connected with specific symptoms [3]. According to World Health Organization (WHO) experts, the term ‘menopausal ailments’ only refers to those that directly result from fluctuations in the hormone system [4]. They include excessive perspiration and hot flushes (vasomotor symptoms) [5–8], urogenital atrophy, and irregular menstruation. However, there is a wide range of other common menopausal symptoms including the following: nervous tension, heart palpitations, headaches, lack of energy [9], insomnia [10–13], depressed mood [14, 15], vaginal dryness, urinary incontinence and sexual concerns or problems [16–18], cognitive symptoms, painful or stiff joints, reduced bone mass [19–20], and hair thinning or loss as well as increased hair growth on other areas of the body (face, neck, chest, and upper back).
Menopausal symptoms can be disturbing, particularly as they occur at a time when women play important roles in society, within the family, and in the workplace. Findings from longitudinal studies have shown that ethnic, geographic, and individual factors affect the prevalence and severity of symptoms [21]. The prevalence of hot flashes and sleep disorders increases during the late menopausal transition and postmenopausal stages whereas vaginal dryness and other sexual problems become more prevalent during the postmenopause than the late reproductive or menopausal transition stages. It is unclear whether depressed mood, urinary control, cognitive functioning, and joint and muscle pains vary across the menopausal transition [6, 22]. Moreover, the findings have highlighted that vasomotor symptoms can be associated with the onset of other disorders and might therefore indicate future health risks in postmenopausal women [23]. The duration and intensity of menopausal symptoms induce women to apply methods aimed at their alleviation. Menopausal hormone therapy (MHT), formerly known as hormone replacement therapy, is the main conventional therapy. The type, form, and dosage of the hormone drugs are decided by a gynaecologist, individually, in relation to the patient’s needs [24]. However, in 2002, the first Women’s Health Initiative (WHI) study showed that MHT increased the risk of coronary artery disease, breast cancer, stroke, and venous thromboembolism in healthy postmenopausal women. The study also found a decreased risk of colorectal cancer, hip fractures, and total fractures with combined hormone therapy [25]. Due to serious side effects, the increasing effectiveness of alternative therapies (AT) in counteracting the experienced symptoms and thus improving the quality of life of menopausal women is highlighted. The nonconventional methods comprise, among others, herbalism [26–28], a balanced diet [29, 30], physical activity [31–33], acupuncture or hypnosis [34, 35], cognitive behavioural therapy, and omega-3 supplements [36]. The advantages of using non-conventional menopausal therapies are more commonly presented in leading journals devoted to the issue of menopause. However, the efficiency of alternative methods is not clear. Although, data from the Study of Women’s Health Across the Nation (SWAN), a multi-site longitudinal study, involving 3018 women aged 42–52 years, indicated a decrease of women’s interest in conventional methods, they are still considered the leading ones among the majority of health care workers and patients [37].
The aim of the study was to assess the prevalence of menopausal symptoms in peri- and postmenopausal women, the frequency of use of hormone therapy and nonconventional methods of alleviating menopausal symptoms, and to analyse their reported health benefits.
Material and methods
Material status and method
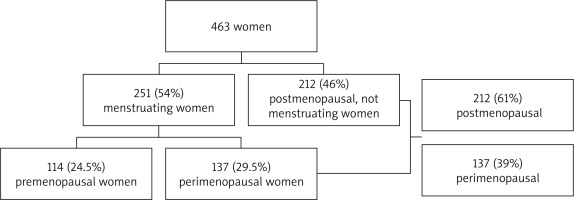
A total of 463 Polish women aged 40–78 years from urban and rural areas of the Lower Silesian and Opole voivodeships were invited to participate in the study. Recruitment took place over the period 2018 and 2019. All women completed a detailed questionnaire, which provided information on reproductive factors, and socioeconomic (place of residence, education level, occupational status, and net income per person/per month in the family) as well as menopausal status. Based on the WHO recommendations, i.e. the date of the last menstruation and occurrence of menopausal symptoms during the examination or in the past, 3 groups were distinguished: women in pre- (24.5%), peri- (29.5%), and postmenopausal (46%) periods (Fig. 1). All peri- and postmenopausal women answered questions about their menopausal symptoms and the type of therapy used (MHT or AT) and their benefits. Premenopausal women were asked about their knowledge of menopausal transition and conventional or AT, and these results were published earlier [38]. Natural menopause was defined according to the WHO as amenorrhoea for at least 12 consecutive months without other obvious reasons. All women who experienced a surgical menopause (i.e. hysterectomy and/or unilateral or bilateral ovariectomy) or were at the premenopausal period (a total of 114 women) at time of enrolment were therefore excluded. Finally, a sample of 349 peri- or postmenopausal women were included in the study: 212 women (61%) aged 50–78 years stated that they had not had any menstruation for at least 12 months, whereas 137 (39%) aged 41–54 years still menstruated (Fig. 1). Both groups comprised women who experienced menopausal symptoms during the study period or in the past. Moreover, all participants were fully informed about the purpose of the study, its anonymity, and the possibility of refusing to participate in the study and gave their consent.
Place of residence was categorized as 1) rural and small urban centre with a population under 50,000, 2) medium-size urban centre with a population between 50,000 and 500,000, and 3) large urban centre with a population over 500,000. The women’s education level was classified as 1) low-level (no education, primary or vocational school education), 2) mid-level (secondary, post-secondary school), and 3) high-level (completed MA studies, continuation of education after university studies – postgraduate studies, second line of studies, doctoral studies, etc.). Occupational status was categorized as 1) inactive and 2) active. Net income per person/per month in the family was described as 1) low (< 1000 PLN/pers.), 2) medium (1000–2000 PLN/pers.), and 3) high (> 2000 PLN/pers.).
Five questions were used to assess the kinds of menopausal symptoms experienced by the women, the type of therapies chosen to alleviate them, as well as the health benefits of applying MHT or AT: ‘Have you ever experienced or do you still experience menopausal symptoms that occur during menopausal transition? If ‘yes’, please tick them on the list below’; ‘Have you ever used or do you still use MHT?’: ‘yes’, ‘no’; ‘Have you ever used or do you still use AT’: ‘yes’, ‘no’; ‘If you applied/apply menopausal hormone therapy, please choose from the list below the area of health benefits (relieve menopausal symptoms, emotional condition, sexual life, physical activity, state of heart & blood vessels, skin condition, condition of bones and joints) you have experienced or still experience’; ‘If you applied/apply alternative therapies, please choose from the list below the area of health benefits (relieve menopausal symptoms, emotional condition, sexual life, physical activity, state of heart and blood vessels, skin condition, condition of bones and joints) you have experienced or still experience’. In addition, a 7-item Likert scale (where 1 means ‘I do not feel any advantages of applying MHT/AT’ and 7 means ‘I feel a very advantageous influence of applying MHT/AT’) was designed to evaluate self-assessed advantages of applying MHT and AT.
Ethical considerations
All procedures contributing to this work complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the 130 Helsinki Declaration of 1975, as revised in 2008.
Statistical analysis
The characteristics of the sample were described using means and SD values for continuous variables as well as frequencies and percentages for categorical factors. In the univariate analyses, the χ2, and 2-tailed independent sample t-Student and Mann-Whitney U tests were used. Moreover, 2 types of logistic regression analyses were undertaken. The first was a univariate logistic regression to calculate the odds ratio (OR) of health benefits in peri- and postmenopausal women applying MHT and AT. The second analysis, a sequential logistic regression (with Bonferroni correction), initially removed the effects of all the other independent variables before testing for the variable of choice. For example, the independent association between the benefits in relieve of menopausal symptoms among peri- and postmenopausal women using MHT was assessed after removing the effect of sexual life, whereas the independent association between benefits in sexual life among peri- and postmenopausal women using AT was assessed after removing the effects of physical activity and skin condition. The analyses were performed using STATISTICA version 13.0 for Windows software.
Results
The mean age of peri- and post-menopausal women was 49.55 (±2.51) and 61.32 (±6.77) years, respectively. Overall, 42.2% of the women came from rural and small urban centres and 71% had a medium or high income level. Almost 42% of perimenopausal women had a high level of education, whereas postmenopausal women tended to have a mid- or a low-level of education (44.8% and 36.3%, respectively). The majority (71.5%) of perimenopausal women were occupationally active, whereas postmenopausal women were mainly inactive (70.8%). The distribution of demographic and socio-economic variables is presented in Table 1.
Table 1
Demographic and socioeconomic characteristics of peri- (n = 137) and postmenopausal (n = 212) women
Prevalence of menopausal symptoms among peri- and postmenopausal women
The most frequently reported menopausal symptoms in perimenopausal women were fatigue (78.8%), mood swings (70.1%), and hot flushes (67.2%) whereas fatigue (75.5%), sleep disturbances (65.1%), and hot flushes (62.3%) were the most uncomfortable symptoms in postmenopausal women (Table 2). Perimenopausal women experienced mood swings (70.1%), headaches (62.8%), and vaginal dryness/itching (53.3%) more often than postmenopausal women, while postmenopausal women experienced aches or stiff joints (47.2%) and heart palpitation (44.8%) more often than perimenopausal women (Table 2). Among 13 symptoms specified in the questionnaire, only 8 (2.3%) women declared at least 11 of them. There was no difference between the mean number of menopausal symptoms reported by peri- and postmenopausal women (6.5 vs. 6.1, respectively, z = 1.202, p = 0.230, not presented).
Table 2
The prevalence of menopausal symptoms among peri- (n = 137) and postmenopausal (n = 212) women
The frequency of using menopausal hormone therapy and alternative therapies in peri- and postmenopausal women
Altogether 45% of the women said they currently or in the past used MHT, whereas for AT it was 27.8%. Postmenopausal women used MHT more often (OR 1.86; 95% CI: 1.20–2.90; p = 0.006) than perimenopausal women, while perimenopausal women applied AT more often (OR 1.73; 95% CI: 1.06–2.76; p = 0.027) than postmenopausal women (Table 3).
Table 3
The frequency of using menopausal hormone therapy and alternative therapies in peri- (n = 137) and postmenopausal (n = 212) women
Health benefits experienced by peri- and postmenopausal women due to menopausal hormone therapy and alternative therapies
Perimenopausal women reported more advantageous influences of using MHT (z = 3.316, p < 0.001) and AT (z = 2.295, p = 0.022) than postmenopausal women (Table 4).
Table 4
The advantages of using menopausal hormone therapy and alternative therapies in peri- and postmenopausal women
| Menopausal status | n | Mean | SD | z | p |
|---|---|---|---|---|---|
| Use of MHT | |||||
| Perimenopausal Postmenopausal | 49 104 | 5.80 5.01 | 0.94 1.39 | 3.316 | < 0.001 |
| Use of AT | |||||
| Perimenopausal Postmenopausal | 46 43 | 5.67 5.09 | 1.12 1.09 | 2.295 | 0.022 |
Perimenopausal women using MHT reported reduced menopausal symptoms (OR 3.01; 95% CI: 0.97–9.32; p = 0.046) and benefits in their sexual life (OR 5.55; 95% CI: 2.64–11.46; p < 0.001) more often than postmenopausal women (Table 5). Moreover, perimenopausal women using AT experienced benefits in sexual life (OR 6.29; 95% CI: 2.28–18.27; p < 0.001), skin condition (OR 5.89; 95% CI: 2.36–14.75; p < 0.001), and physical activity (OR 2.88; 95% CI: 1.25–6.64; p = 0.014) more often than postmenopausal women (Table 6). After taking into consideration all health benefits experien- ced by the women it appeared that sexual life (OR 5.01; 95% CI: 2.37–10.61; p < 0.001) remained significant among perimenopausal women using MHT (Table 5).
Table 5
The results of univariate and multivariate (sequential) logistic regression analyses to predict health benefits experienced by peri- and postmenopausal women using menopausal hormone therapy
Table 6
The results of univariate and multivariate (sequential) logistic regression analyses to predict the health benefits experienced by peri- and postmenopausal women using alternative therapies
Discussion
Menopausal symptoms experienced by women vary widely, and a lot of women experience severe symptoms, which may impair their quality of life. Although there is substantial evidence of the advantages of MHT, a growing interest in complementary and AT is well-known as well. A comprehensive assessment of the effects of using MHT and AT among peri- and postmenopausal women is lacking. The current study demonstrates the prevalence of menopausal symptoms in peri- and postmenopausal women, the frequency of use of hormone therapy and nonconventional methods of alleviating menopausal symptoms, and the health benefits due to MHT and AT use in regard to peri- and postmenopausal women.
The prevalence of menopausal symptoms among peri- and postmenopausal women
Several studies have confirmed an association between psychological symptoms, somatic complaints, and menopausal status [9, 19, 39–54], but cross-cultural differences indicate that reporting symptoms are not universal. What is more, there is no consistency regarding which symptoms are the most prevalent among peri- and postmenopausal women. Hunter et al. [39] studied 682 women aged 45 to 55 years in England and indicated that vasomotor symptoms, sexual functioning, and sleep problems were the most prevalent in postmenopausal women, whereas depressed mood was more prevalent in peri- and postmenopausal women compared with premenopausal women. In another study conducted on 8623 Australian women aged 45–50 years, the most commonly reported symptoms were headaches, back pain, stiff joints, tiredness, and difficulty sleeping. Perimenopausal women were more likely than premenopausal or postmenopausal women to report these symptoms. Hot flushes and night sweats were more common among postmenopausal women [40]. In a survey of 148 Swedish women, it appeared that only vasomotor symptoms and joint pain were associated with menopausal status [41]. Data from 1572 British women confirmed that vasomotor symptoms were found to be strongly related to changes in menopausal status with increases being observed as women move through the menopause. Psychological symptoms were more strongly associated with current life events and difficulties than with menopausal status [42]. Other studies based on 1743 Australian and Japanese women aged between 40 and 60 years showed that vasomotor, psychological, and somatic symptoms decreased after menopause in Australian women, with only sexual symptoms continuing. In Japanese women, somatic, psychological, and sexual symptoms remained high after menopause [43]. Another study conducted on 1069 Japanese women aged 40–60 years indicated that the most frequent symptom was general fatigue, reported by 88.2% of the women. What is more, the prevalence and severity of hot flushes (and sweats) were slightly higher in peri- and early postmenopausal women than in pre- and late postmenopausal women [44]. The cross-sectional portion of the SWAN provided the opportunity to examine the prevalence of various symptoms by menopausal status in a multi-ethnic and multisite sample of middle-aged women from across the United States [9]. Hot flushes or night sweats increased considerably from early perimenopause to late perimenopause (38–55%) and declined noticeably from late perimenopause to postmenopause (55% vs. 44%, respectively). Psychological symptoms remained the same or slowly decreased in prevalence among women in late perimenopause compared with postmenopause. A cross-sectional study of 1427 women from Finland aged 45–64 years found that mental symptoms dominated the list of reported symptoms during the menopausal transition [19]. Occurrence of pains and vasomotor problems was equally frequent among Brazilian women [45]. Research carried out on 3147 women aged 40–60 years in Shanghai, China revealed that menopausal symptoms were the most common (81.7%) among perimenopausal women. The top 3 reported symptoms were fatigue (38.08%), hot flushes and sweating (33.65%), and joint ache (28.81%) [46]. Another study conducted among 400 women (40–60 years) from Haryana, India showed that the prevalence of menopausal symptoms was 87.7%. The majority of the study subjects had anxiety (80%), followed by physical and mental exhaustion (71.5%), sleep problems (61.2%), and irritability (60.7%). Hot flushes were reported in 36.7% [47]. A population-based survey carried out on a representative sample of 495 Singaporean women aged 40–60 years indicated that classical menopausal symptoms such as hot flushes (17.6%), vaginal dryness (20.7%), and night sweats (8.9%) were less commonly reported than somatic symptoms. The most prevalent symptom reported was low backache with aching muscles and joints (51.4%). There was no correlation between menopausal status and somatic symptoms or depression [48]. In a sample of 1030 Turkish women aged 40–59 years, it appeared that the most frequently experienced menopausal symptoms were feeling tired and worn out (79.2%), aches in the muscles and joints (79.1%), and low backache (77.8%), whereas the least experienced symptom was an increase in facial hair (28.3%) [49]. Data from a nationally representative sample of 4402 US women aged 40–65 years indicated that the prevalence of vasomotor symptoms was 79% in peri- and 65% in postmenopausal women [50]. Another study conducted on 102 US women aged 45–65 years confirmed that the most common menopausal symptoms were hot flushes (40%), night sweats (17%), insomnia (16%), vaginal dryness (13%), mood disorders (12%), and weight gain (12%) [51]. Previous research carried out on a sample of 244 postmenopausal women from Poland showed that the frequency and intensity of psychological symptoms were significantly higher than vasomotor and somatic ones [52]. Similar results were obtained by Kupcewicz et al. in a sample 334 Polish nurses aged 45–55 years, where more severe complaints in the subscales of psychological than somatic and vasomotor symptoms were reported [53]. The present study indicated that the most frequently reported menopausal symptoms were fatigue (78.8% in peri- and 75.2% in postmenopausal women), mood swings (70.1% in perimenopausal women), hot flushes (67.2% in peri- and 62.2% in postmenopausal women), and sleep disturbances (65.0% in postmenopausal women). What is more, perimenopausal women experienced mood swings (70.1%), headaches (62.8%), and vaginal dryness/itching (53.3%) more often than postmenopausal women, while postmenopausal women experienced aches or stiff joints (47.2%) and heart palpitation (44.4%) more often than perimenopausal women.
The frequency of using menopausal hormone therapy and alternative therapies
Menopausal hormone therapy seems to be the most intuitive and effective way of improving menopausal symptoms such as hot flashes, sweating, and emotional changes. However, almost 2 decades after the presentation of the first results of the WHI study, it has been established that the demand for using nonconventional/AT (herbalism, acupuncture, yoga, aromatherapy, massage, relaxation, cognitive behavioural modifications, antidepressants, antiepileptics, antihypertensives, regular physical activity) has increased substantially [54]. Data from 696 postmenopausal Belgian women aged 45–60 years showed that MHT was used significantly more often by French-speaking women (32%) than by Dutch-speaking women (9%). The alternatives to MHT had a high satisfaction rate among users. Relaxation techniques, regular physical activity, acupuncture, and avoiding stress had satisfaction rates similar to that with MHT [16]. Another cross-sectional population-based study of 749 Brazilian women aged 45–60 years indicated that among all the women included, 19.5% reported current or previous MHT use [55]. The study of 4721 Turkish women aged 40–65 years revealed that 73.6% of women in the menopausal period were using complementary and alternative medicine (herbal supplements, dietary supplements, mind-body and religious practices) and 72% of them stated that the method used was effective [56]. A lower percentage (33.5%) of women using complementary and alternative medicine was noted among women aged 45–65 years from Bologna [57]. Previous research from 2004 on a nationally representative group (HORTPOL 2002) of 1544 Polish women aged 18–87 years showed that only 12% of the women applied a MHT [58]. Whereas a study from 2005 comprised 1083 women aged 45–54 years revealed that only 7% of the participants admitted using MHT [59]. Other studies (SOPKARD and GDYNIAKARD) conducted on a sample of 586 Polish women aged 50 years (317 pre- and 269 postmenopausal) indicated that 29% of women were current users of MHT. What is more, most of the women pointed out the improvement of wellbeing as an advantage of MHT use [60]. The present study demonstrated that, contrary to AT (27.6%), MHT was the more frequently used therapy, chosen by 45% of the women. Moreover, perimenopausal women used AT more often than postmenopausal women, whereas postmenopausal women used MHT more often than perimenopausal women.
The health benefits of menopausal hormone therapy and alternative therapies
Current literature reports that MHT remains an effective therapy for vasomotor symptoms and genitourinary syndrome of menopause as well as arthralgia and muscle pains, sleep disturbances, and skin condition. Individualized MHT may improve both sexuality and overall quality of life. In addition, MHT is effective in preventing the acceleration of bone turnover and the bone loss associated with the menopause [61–65]. A cross-sectional observational study conducted on 210 Polish women between the ages of 45 and 55 years demonstrated that those using MHT had higher body esteem during sexual activities and better sexual function (the Changes in Sexual Functioning Questionnaire – CSFQ) [66]. Another study on 1239 women from the northwestern, central, and northern parts of Poland indicated that the highest efficacy in terms of relief from menopausal symptoms, such as shortness of breath, flushing, or sweating, was observed for a combined MHT and selective antidepressant therapy. Nevertheless, phytoestrogen therapy was also highly effective [67]. From the search 27 studies (16,393 women) indicated that MHT treatment with oestrogens alone or in combination with progestogens was associated with a small to moderate improvement in sexual function, particularly in pain, when used by women with menopausal symptoms or in early postmenopause [68]. In the current study perimenopausal women using MHT experienced reducing menopausal symptoms and benefits in their sexual life more often than postmenopausal women. After taking into consideration all health benefits experienced by the women it appeared that sexual life remained significant among perimenopausal women using MHT.
Nonconventional therapy seems to be a noninvasive, well-tolerated, and most often simple option, and thus may be a promising alternative to hormonal treatment, particularly for women with diagnosed contraindications for applying conventional therapies. Alternative therapies can help prevent and treat menopausal symptoms such as skin aging, osteoporosis, cardiovascular disease, sleep disturbances, and cognitive disorders [69–72]. A general improvement of AT in sexual life (orgasm, vagina moisturising, and pain reduction during intercourse) among postmenopausal women is also well-known [73]. A randomised, triple-blind study of 80 postmenopausal women aged 50–60 years revealed that Aphrodit capsule use (a herbal supplement consisting of ginger, saffron, cinnamon, and Tribulus terrestris) was effective in reducing physical, mental, and genitourinary menopausal symptoms [74]. The present study indicated that perimenopausal women using AT experienced benefits in sexual life, skin condition, and physical activity more often than postmenopausal women.
Limitations
The current study has also some limitations. First, we lacked information on the age of initiation as well as the duration of MHT or AT usage. Moreover, women were asked to provide some information related to their memory such as symptoms they experienced in the past or in previous weeks/months, menopause age, and regularity of menses, hence recall biases were inevitable. The collected data were based on a self-reported questionnaire and the women’s declarations.
Conclusions
This study indicates that the most common symptoms connected with the menopausal transition are mental ailments. In order to prevent them, the women more frequently applied MHT in comparison to alternative methods, with postmenopausal women using MHT more often than perimenopausal women. Satisfaction was found with both conventional and alternative treatments for the relief of menopausal symptoms. The women who used MHT more often reported benefits in sexual life, whereas the women who used alternative methods reported benefits in relation to sexual life, skin condition, and physical activity.