Biliary disease and cholecystitis remain one of the most significant surgical challenges. Over 1,000,000 cholecystectomies are performed in the US every year [1, 2], and over 50,000 in the UK [3]. While minimally invasive laparoscopic cholecystectomy (LC) has afforded great advantages over open cholecystectomy, reducing variability and improving outcomes remains a challenge [4, 5]. It is only recently that operative classifications and grading of cholecystitis have been published [6]. LC related peri-operative complications, while infrequent may result in potential readmission to hospital [7]. Understanding the process of readmission, its prevalence and potential associated factors would be important in improving the delivery of care for patients undergoing biliary surgery. A number of key publications on readmission following cholecystectomy have been reported but to date, to our best knowledge, no meta-analysis has been published [8–11]. The aim of this study was to evaluate the prevalence of readmission after LC and if possible, factors predisposing to it.
METHODS
Search strategy and study eligibility
An ethically approved, PROSPERO registered meta-analysis of all published English articles pertaining to unplanned readmission following LC was undertaken at Letterkenny University Hospital searching PubMed, Scopus, Web of Science and Cochrane Library electronic databases over a 5-and-a-half-year period from January 2013 to June 2018. The search terms ‘readmission’, ‘laparoscopic cholecystectomy’, ‘outcome’, ‘return’, ‘readmitted’ ‘rates’, not ‘open laparoscopic cholecystectomy’ and not ‘conversion to open’ were used in combination with Boolean operators AND or OR. The primary outcome of interest was unplanned readmission of patients post index LC.
The method of analysis and inclusion criteria were specified in advance to avoid selection bias and documented in a protocol which was prospectively registered and published with the International Prospective Register of Systematic Reviews (PROSPERO) on 25/07/2018 (ID: CRD42018104960). This meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
Studies were included in the systematic review if the following criteria were met; studies that involved LC which reported readmission rates post-laparoscopic cholecystectomy, and observational studies and randomized control trials whose full text articles were available in the English language.
Studies were not included if they were systematic reviews, meta-analyses, case reports, letters or protocols, studies that did not report key outcomes, related to interval laparoscopic cholecystectomies, obstetric and paediatric studies, and those which data was inadequate for interpretation via meta-analysis. Publications relating to open cholecystectomy were not included.
Definitions
Hospital readmission was defined as any unplanned readmission to hospital within 30 days of discharge following LC. When the timing of readmission was not defined in the study it was assumed to be within 30 days of discharge. Readmission rate was expressed as the number of readmissions as a percentage of the overall number of laparoscopic cholecystectomies performed. Where reported, causes of readmission and contributing factors were recorded.
Data extraction and quality assessment
The descriptive and quantitative data from the screened studies were extracted by the same reviewer and were entered into a computerized spreadsheet for analysis. Once the data extraction was completed a quality assessment tool was chosen to determine the studies with highly rated methodologies suitable for inclusion in the final analysis. The tool chosen for the quality assessment was the Methodological Index for Non-Randomised Studies (MINORS) criteria [12]. This tool is designed for the quality assessment of comparative and non-comparative surgical studies using a 3-point scale (0 – not reported, 1 – reported but inadequate, 2 – reported and adequate) on eight items for non-comparative studies and twelve items for comparative studies. The global ideal score being 16 for non-comparative studies and 24 for comparative studies.
Quality assessment was performed independently in a blinded standardised manner by two reviewers. Disagreements between reviewers were resolved by discussion between the two review authors (CM, DF). If no agreement could be reached, a third reviewer (JL) analysed the publication and decided on inclusion. Comparative studies with a MINORS score of > 15, and non-comparative studies with a MINORS score of > 10 were included in the final analysis.
Statistical analysis
The overall readmission rate was based on the cumulative rates of readmission in included studies. Risk factors and their potential relationship to readmission rates was analysed using odds ratio (OR) and 95% confidence intervals (CI) for each possible risk factor was calculated, along with the P-value with < 0.05 representing statistical significance. The Mantel-Haenszel method and fixed-effects models were used due to low heterogeneity. Hete-rogeneity was assessed using the I2 statistic where a value greater than 75% was considered high and a less than 25% was considered low.
RESULTS
This meta-analysis reviewed 3832 articles, 67 meeting inclusion criteria, and 44 [8–10, 13–52] were finally enrolled after applying the MINORS score. Figure 1 shows the modified PRISMA flowchart for identification and inclusion of relevant papers. Twenty-three studies were excluded from the meta-analysis; 10 papers were deemed low quality [53–61] and 13 papers did not provide readmission rates specific to LC [62–74].
Readmission rate
A total of 1,573,715 LC were reported, with 52,628 readmissions within 30 days. The overall readmission rate was 3.3%, ranging from 0% to 11.7%. Reported readmission rates for all studies are shown in Figure 2.
The difference in readmission rate did not differ between large studies (sample size of > 1000 patients, see Figure 3) and small studies (sample size of < 1000 patients, see Figure 4), with an average of 3.3% in both groups.
Studies analysed were from 25 countries, with 20/44 carried out in Europe (total cohort 30,583) and 8/44 carried out in North America (total cohort 1,257,910) with readmission rates of 7.7% and 3.6% respectively.
Out of the 44 studies included, 12 reported a readmission rate of ≥ 5%, and 32 studies reported a readmission rate of < 5%. Studies reporting a readmission rate of ≥ 5% had an average cohort size of 15,000, whereas studies reporting a readmission rate of < 5% had an average cohort size of 44,000. There were three studies that reported a readmission rate > 7%; these include Vohra et al. [43] based in the UK and Ireland (7.1%), Fuks et al. [19] based in France (9.5%) and Nielsen et al. [31] based in Denmark (11.7%).
Causes of readmission
Of the 44 studies, 25 reported the reasons for patient readmission post-LC, accounting for only 4,002 out of 52,628 readmissions. Causes of all readmissions were reported in only 19 of these studies, with the remaining 6 studies partially reporting. Rosero et al. [8] provided 3,712 out of the 4,002 reasons for readmission, and reported on day case procedures in the USA. For this reason, Figure 5 shows reasons for readmission reported in Rosero et al. [8] and those reported in all other studies (which consisted of a mix of both day case and inpatient procedures) separately. Surgical complications accounted for 56% of reported reasons for readmission, predominantly bile duct complications (46%), other (16%), nausea and vomiting (11.8%) and bleeding (8%). Bile duct complications reported by Rosero et al. [8] included bile duct obstruction in 995 cases accounting for 21.3% of their readmission. Nine hundred and three of these cases were treated with endoscopic procedures. Bile duct injury accounted for 30 cases. Bile leak was not reported as a complication in Rosero et al. [8] However, it was reported in a number of other studies as a cause for readmission and accounted for 32 cases [9, 10, 20, 22, 34, 39, 41, 42, 50–52, 75]. Pain (16%), surgical site occurrence (14%) cardiorespiratory complications (9%), and unrelated medical (6%) account for the remainder.
Risk factors associated with increased readmission
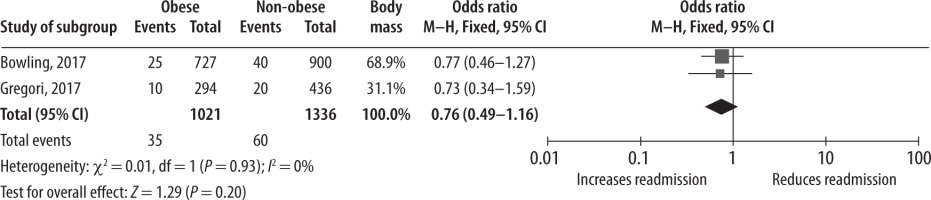
None of the risk factors analysed for readmission post-LC were found to be significant. Obesity (BMI > 30) was the only pre-operative patient factor for readmission analysed and was not statistically significant [20, 50] (OR = 0.76, CI = 0.49–1.16, P = 0.20) (Figure 6).
Surgical factors analysed included single port LC vs. four port LC [13, 29, 42] (OR = 1.27, CI = 0.83–1.96, P = 0.27) (Figure 7), and day case LC vs. inpatient LC [17, 37] (OR = 0.50, CI = 0.16–1.53, P = 0.23) (Figure 8).
DISCUSSION
This meta-analysis reviewing 44 publications dealing with over 1.5 million patients undergoing LC identified that, on average one in thirty patients are readmitted within 30 days. This reflects the findings of Tang et al. [75], in their meta-analysis comparing day case and inpatient LC, which reported a mean post discharge readmission rate of 2.4%, and an in-patient admission rate of 13.1%. Readmission rates were not found to be statistically significantly different between large studies and small studies (Figures 3 and 4), nor whether the surgery was undertaken in Europe [31, 50] or North America [8, 33].
Readmission has become a quality indicator in the delivery of medical care [70, 75]. This relates to both the inconvenience to patients, the cost, resource utilisation and the associated morbidity and potential mortality. Cholecystectomy itself is one of the commonest procedures undertaken with over one million cholecystectomy’s performed in the US annually [1, 2]. A readmission rate of 3% would have significant impact on utilization of resources, accounting for potentially 30,000 patients readmitted annually in the US alone, which equates to almost all index cholecystectomies performed in the UK. One of the challenges relating specifically to cholecystectomy is the variation that occurs both within patient cohorts and also the variation in actual operative findings.
Understandably, complex medical patients with increased co-morbidities are potentially more likely to have adverse outcomes and either prolonged hospitalization time or increased readmission rates. Attempts at defining operative grading have only recently been achieved. Sugrue et al. [6] in 2015 reported one of the first operative scoring systems in an attempt to define benchmarks for streamlining outcome analysis. Since then other scoring and grading systems have been reported including the AAST [76] and Cairns [77] scoring systems. This may aid in the comparison of patients’ operative severity and grade.
Increasingly, health insurance companies will penalize hospitals where readmissions have occurred. It is therefore important to have common denominators in determining acceptable or anticipated outcomes versus excess variability that is no longer acceptable. Some of the studies in this group had high readmission rates approaching 12%. The Surgical Variance Report 2017 [78] by the Royal Australasian College of Surgeons, reported a readmission rate of 8% with marked variation.
Limitations of this meta-analysis include the exclusion of papers not providing adequate data, most commonly due to failure to specify if readmission was following LC or open cholecystectomy. Authors of these studies were not contacted to obtain this data. A second limitation is, when not specified by studies, readmission was assumed to mean readmission to hospital within 30 days of discharge. The reasons for readmissions unfortunately, are not widely reported. This indicates the need to have a robust international data reporting system for biliary disease. These modules could be built into existing inpatient surgical registries or emergency surgery registries. Coccolini et al. [79] has proposed a mechanism whereby the World Society of Emergency Surgery (WSES) would develop a worldwide emergency general surgery formation and evaluation project. This will determine common benchmarks for training and education programmes worldwide in an effort to standardize management, improve outcomes and ultimately save lives. At one of the world’s first emergency surgery performance improvement programs in emergency general surgery [80] key performance indicators for LC did not include readmission rate.
The causes for readmission identified in this meta- analysis predominately related to biliary complications. Nausea, vomiting and peri-operative pain were not infrequent followed by surgical site occurrence. Reported reasons for readmission come from day case procedure cohort studies [8]. In the Rosero et al. [8] series, many readmissions are a result of the underestimation of post-operative pain expected in this procedure in an outpatient setting [81]. An aggressive procedure-specific multimodal analgesia and concomitant antiemetic therapy regimen should be determined for use both immediately following surgery and following discharge home to address this potential cause for readmission [82]. Rosero et al. [8] discovered several risk factors for increased readmission using hierarchical mixed regression analyses. These included co-morbidities such as chronic renal failure, chronic pulmonary disease, liver disease and cancer, and patient demographics such as male sex, increasing age, non-Hispanic white race/ethnicity and non-private insurance type. They also identified surgical risk factors for readmission, which included the type of procedure and the indication for surgery. Patients presenting with acute cholecystitis had a 30% higher chance of being readmitted in comparison to those presenting with chronic cholecystitis. Similar findings are described by Giger et al. [83]. Also, patients undergoing surgery on a weekend were also associated with significantly increased readmission rates. Interestingly, the risk of readmission was reduced when intra-operative cholangiogram was implemented by about 15% which is supported by the findings of Halawani et al. [29] following analysis of the National Surgical Quality Improvement Program database (NSQIP). Due to the potential seriousness of biliary complications, it begs the question of the current global approach to intra-operative cholangiography and single stage bile duct clearance. A recent meta-analysis by Pan et al. [84] found performance of intra-operative cholangiography to have superior outcomes in managing cholecysto-choledocholithiasis.
Attempts to improve safety and reduce biliary complications including identification of the critical view of safety, the use of Rouviere’s sulcus as a landmark and the use of intra-operative cholangiography have not been uniformly adapted. They are prone to misinterpretation and false reporting. Obesity was not significantly associated with readmission in this meta-analysis, which may indicate the need to have more robust gradings for different BMI categories – a BMI > 30 does not fit all. This study cannot overcome the limitations of the original studies. Obesity is a continuous outcome; however it is reported as a dichotomous outcome in original studies. This “obesity paradox” is currently a widely discussed issue in surgical literature. While the categorisation of continuous variables simplifies outcomes for presentation of results, for example in tables, it is unnecessary for statistical analysis and reduces the power of the statistical analysis as a result [85, 86].
We identified a baseline rate for readmission with significant variation. This suggests that there is an onus on the surgical community to help standardize the metrics of cholecystectomy.
CONCLUSIONS
While overall readmission following LC is uncommon, there are opportunities to reduce this through attention to operative strategies including use of intra-operative cholangiography and attention to post-operative analgesia and reduction in nausea. Focusing on high risk groups, including acute cholecystitis patients and surgery performed at weekends could enhance outcomes. Some crucial data concerning perioperative course and outcomes in cholecystectomy should be implemented into large international registries in order to improve our understanding of potential risk factors for complications.