Dear Editor,
The interscalene groove is the space between the anterior and middle scalene muscles which extends from the lateral head of the sternocleidomastoid muscle at the level of the C6 tubercle to the first rib where the scalene muscles are attached [1]. The contents of the interscalene groove include the brachial plexus roots at the upper level which converge to form trunks at a lower level. The interscalene block covers most of the brachial plexus, sparing the ulnar (C8–T1) nerve. It is a useful block for distal clavicle, shoulder, and proximal humerus procedures [1].
Interscalene block is performed by injecting the drug into the interscalene groove. There are no clear cut guidelines regarding the exact site of drug deposition – roots or trunks – even during ultrasound (US)-guided interscalene block. Though there are numerous studies, none of these compare two sites of injection (at the level of the root or trunk) in terms of success rate of distal analgesia (forearm and hand), ease, and complications.
Madison et al. [2] described two-point drug injection during interscalene block to evaluate the analgesic effect at the ulnar part of the forearm and hand. The first point was between the deepest and next-deepest brachial plexus root/trunk; this was followed by redirection of the needle so that the needle tip was placed between the most superficial and next most superficial brachial plexus root/trunk. However, their results do not support the two-level deposition of local anaesthetic (LA) at the root/trunk level to provide hand and forearm anaesthesia.
As per our experience, it should be better to inject the drug at a site after formation of the upper trunk where C5 and C6 roots merge (Figure 1, panel C). The benefits of injection at a site after formation of the upper trunk include:
FIGURE 1
A) Sonoanatomy of interscalene block at C6 level (white arrows: anterior tubercle, green arrow: posterior tubercle, yellow arrow: phrenic nerve). B) Sonoanatomy of interscalene block at C7 level (before fusion of C5 and C6 root). C) Sonoanatomy of interscalene block after formation of superior trunk. MSM – middle scalene muscles, ASM – anterior scalene muscles, SCM – sternocleidomastoid muscle, VA – vertebral artery
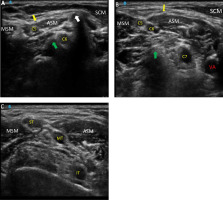
Sparing of phrenic nerve blockade, as it moves away from the C5 root (Figure 1, panel B).
Avoiding the possibility of needle redirection, which is not recommended due to greater likelihood of intraneural injections.
Avoiding dorsal scapular nerve injury. This nerve is mainly derived from the 5th cervical nerve root and emerges before the formation of the trunk. Similarly, blockade of the long thoracic nerve can be avoided as it arises from the anterior branches of the 5th, 6th, and 7th cervical nerve roots and emerges before the formation of the trunk [3].
The scalene muscles originate from the tubercles of C3–C6 (anterior scalene) and C2–C7 (middle scalene). There is progressive increase in the muscle belly as we scan from the root down to the trunk level (Figure 1, panel A to panel C).
Anatomy of the US-guided interscalene groove is more defined at a lower level (at the level of the trunk), which makes the identification of the trunks easier for novice practitioners [4].
There is no anterior tubercle on the C7 transverse process, so no anterior interscalene muscle is situated medial to the C7 root; this may increase the likelihood of vertebral artery puncture whenever the needle is directed to the C7 root for its separate blockade (Figure 1, panel B).
The C8 and T1 root is located very deep when keeping the US probe at C6 or C7 tubercle level, so it is easy to block the inferior trunk by directing the needle than the C8 and T1 nerve root.
Hence for surgery of the distal cla-vicle, shoulder, and proximal humerus it is better to target the interscalene groove at a site distal to the fusion point of C5 and C6 (Figure 1, panel C). Injecting 5 mL volume of the LA is sufficient to block upper trunk divisions and provide sensory analgesia for arthroscopic shoulder surgery. Superior trunk block with 5 mL of 0.5% ropivacaine causes less hemidiaphragmatic palsy when compared to the interscalene block with 15 mL of 0.5% ropivacaine injected between the C5 and C6 roots [5]. A limitation of the above- described technique may be its inability to be used in patients with anatomi-cal variations of the brachial plexus. More research is required to compare the two sites of injection at the level of the root and at the level of the trunk during US-guided interscalene block.




