Adenoid cystic carcinoma (ACC) is a rare type of cancer characterized by low malignancy, average metastasis potential and a relatively good prognosis. It occurs most often within the head and neck area. Within the respiratory tract, it most commonly occurs in the trachea or main bronchi. It originates from the glands located under the mucous membrane. It occurs more often in females (60%), and has no confirmed connection to smoking [1]. Common symptoms of ACC located within the respiratory tract are: breathlessness, productive cough, with or without blood spitting, weakness and decrease in effort tolerance.
A woman, 57 years old, was treated for bronchitis for couple of months without result. Chest X-ray indicated the opacity of the medial and lower lung field.
The patient was directed to the Pulmonology Department, where CT was performed, showing a tumour of 12 × 21 mm located in the main left bronchus, with almost a complete left lung atelectasis (Figure 1).
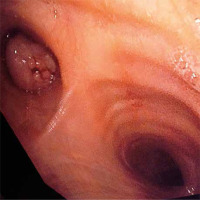
A flexible bronchoscopy showed a smooth, pearl-yellow tumour entirely enclosing the lumen of bronchus and located 1.5–2 cm from the main carina, with a stalk on the medial bronchus wall (Figure 2).
The examination of the histological specimen collected from the affected area showed adenoma bronchi. The patient was directed to the Thoracic Surgery Clinic for rigid bronchoscopy and endobronchial resection of the tumour. It was almost entirely removed. There were no complications following the procedure and the patient was discharged in good condition. The final histopathology result showed adenoid cystic carcinoma, grade 2 (tubular and cribriform structures detected within the tumour area).
Due to the result, further oncological treatment had to be planned, as tumour resection was not radical. 18-FDG PET/CT scan did not show any spread of the cancer; 11 weeks after the resection, flexible bronchoscopy with autofluorescence was performed. In the medial area of the left bronchus wall, about 20 mm from the carina, a submucosal infiltration of about 15 mm, illuminating in autofluorescence imagining (AFI), was diagnosed; the distal section of the main bronchus free from infiltration was 7 mm.
The patient was qualified for segmental resection of the main left bronchus and informed beforehand that the procedure may result in left pneumonectomy, to which the patient consented.
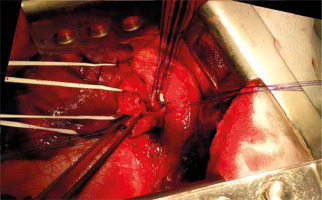
A left posterolateral thoracotomy was performed in order to guarantee good visibility of the surgical field. The intercostal muscle was secured for bronchoplasty. The left pulmonary artery, both pulmonary veins and the main bronchus up to the carina were prepared and hung on rubber guy-ropes. 4L, 5, 6, 7, 8 and 11 group lymph nodes were taken out. About 2 cm from the main carina, a small tumour infiltrating through the wall of the main left bronchus was detected. The main bronchus was cut off around 10 mm from the carina and around 5 mm from the division of the main bronchus. Simple interrupted stitches were put on both stumps and then knotted (Figure 3). Previously prepared intercostal muscle was fixed on the stitch line.
The patient’s condition after the operation was good; flexible bronchoscopy was performed, showing a broad clear anastomosis with a small rotation of the left bronchial tree to the right side.
Final histopathology confirmed adenoid cystic carcinoma, low grade with mitotic index: 0/10 HPF. Cancer infiltrations within the area of 1.2 cm diameter reached the radial margins of the dissected bronchus. Margins proximal and distal were above 1 cm. A fragment of the bronchus of 4.5 cm in length and 2.5 cm in diameter was examined.
Because of the final histopathology result, the patient was not qualified for adjuvant treatment. Instead, the patient showed up for regular follow-up visits; healing of the wound was normal and pain within the operated area ceased after 6 weeks. Twenty weeks after the surgery, flexible bronchoscopy with autofluorescence was performed and it showed clear, broad anastomosis with no reoccurrence both in white light (Figure 4) and in autofluorescence.
CT scan done every 6 months after surgery showed no evidence of local recurrence or disease spread in 3 years’ follow-up.
Initially the patient was histopathologically misdiagnosed with bronchial adenoma. Such a misdiagnosis may occur when sample material is limited, since adenoid cystic carcinoma stems from submucosal glands. The correct diagnosis was possible only due to the immunohistochemical results. After the diagnosis, a PET/CT with 18-FDG was performed as its use is diagnostically confirmed in the cases of ACC. As any remote lesions in the patient were ruled out, and other ontological therapies considered, a radical surgical approach was adopted. Due to its central location and specific biology, adenoid cystic carcinoma is very often a source of many a debate on the best possible method of treatment. It is characterized by low chemical sensitivity, and high radio sensitivity, as well as good effects of surgical treatment. Maziak et al. [2] observed relatively long survival times in patients who underwent a radical microscopic resection. They also pointed out that the intraoperative assessment affects up-staging, and therefore forces one to leave cancer within the incision line when radical resection is technically impossible. Similar effects of the treatment were indicated among 135 patients: 5- and 10-year survival rates of 52% and 29% of those operated on, and only 33% and 10% in non-surgical patients, even though 40% of the patients had positive surgical margins [3].
Radiotherapy within the area of the trachea and main bronchi may cause complications, the most common of which is narrowing of the respiratory tract; however, the smaller the radiated area, the greater the risk of the complication [4]. Nonetheless, surgical treatment of the central lesions requires a very detailed pre-surgical assessment, particular skills of the surgical team as well as very careful planning of the surgery while taking into account all the possible complications. In our patient, because of the tumour location shown in the CT scan as well as because of the endobronchial assessment with autofluorescence, we decided to perform a segmental resection of the upper main left bronchus. Such surgery is regarded as technically difficult, but it has good results in cancerous as well as post-inflammatory or post-traumatic changes [5]. Our case seems to confirm that thesis so far.