Transcatheter aortic valve implantation (TAVI) is an established method of treatment of severe aortic stenosis (AS). Studies show that up to 50% of patients undergoing TAVI have concomitant coronary artery disease, which should undergo percutaneous coronary intervention (PCI) [1]. However, the precise optimal timing of PCI in these patients has not been established yet. European Society of Cardiology guidelines state that PCI and TAVI can be undertaken as single or combined procedures, depending on the clinical situation [2]. Each approach – before, during and after – has its strengths and weaknesses, so the decision lies with the operative team and Heart Team [1].
We present a combined intravascular procedure of TAVI and PCI of the left anterior descending artery (LAD).
An 85-year-old man with chronic heart failure with severe AS, abdominal aorta aneurysm (42 mm diameter), cardiac resynchronization therapy with an implanted defibrillator device, hypertension, hyperlipidemia, diabetes mellitus type 2 and chronic kidney disease was referred to our hospital from cardiac surgery outpatient unit, due to severe dyspnea (stage III/IV in the New York Heart Association Classification) and chest pain with ST segment depression on ECG in leads V2-V6, combined with elevated troponin T levels, reaching 0.058 ng/ml.
Transthoracic echocardiography (TTE) showed severely depressed left ventricle ejection fraction (LVEF) to 18% and severe AS (aortic valve area 0.8 cm2, mean gradient 21 mm Hg, peak systolic velocity 3 m/s – low flow, low gradient AS). There was also akinesia of the infer-septal and inferior wall due to scar tissue as well as overall hypokinesia of other walls. After initial stabilization, due to non-ST segment elevation myocardial infarction coronary angiography was performed, showing 90% stenosis in the proximal segment of the LAD (Figure 1 A).
Figure 1
A – Coronary angiography showing severe lesion of the proximal left descending artery (LAD) (white arrow). B – Computed tomography scan of aorta with massive calcifications on aortic valve and calcium score 4000 AU (white arrow). C – Final result after revascularization of LAD with drug-eluting stent (white arrow). D – Final result of TAVI procedure with Evolut 29 Pro+ bioprosthetic valve (white arrow)
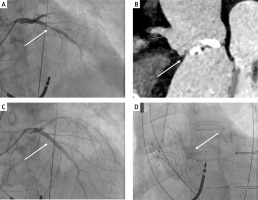
Computed tomography angiography scan with calcium scoring confirmed severe AS with a calcium score of 4000 AU and the anatomy was favorable for TAVI in terms of valve sizing and femoral access (Figure 1 B). The patient was presented at the Heart Team meeting and scheduled for simultaneous PCI of the LAD due to clinical indications with subsequent TAVI for severe aortic stenosis.
The procedure was performed under local anesthesia via the femoral artery after gaining a large bore access. First, PCI of the LAD included balloon predilatation (2.5 × 15 mm) with subsequent drug-eluting stent implantation (4.0 × 24 mm) with an optimal result (Figure 1 C). Secondly, the patient underwent a successful TAVI procedure, with Evolut Pro+ 29 mm (Medtronic, USA) (Figure 1 D). On the following day TTE revealed improvement of LVEF to 25% with trace perivalvular leak and a maximal gradient of 4 mm Hg. The patient was discharged home in overall good condition 4 days after the procedure.
The simultaneous approach for our patient was extremely effective. In the literature some studies suggest that it can result in fewer major adverse cardiac events during the index admission [3]. As more and more cases will be performed as a combination of various procedures, the need for clear guidance will be required in the future [4].








