Quadruple valve endocarditis is a hazardous and potentially lethal condition [1]. The surgical treatment has been published in very few reports; therefore, it is hard to deduce the appropriate treatment strategy for this rare condition.
We report the successful surgical treatment of quadruple valve endocarditis in a patient with heart failure.
A 58-year-old male was admitted to our institute due to symptoms of heart failure (NYHA class III–IV) and fatigue. Medical history revealed hypertension, diabetes mellitus, and obesity. The patient was hospitalized in the general hospital a few months earlier due to prolonged fever and exhaustion. Computer tomography revealed massive pneumonia of the right lung treated with Azithromycin due to penicillin allergy. After hospital discharge the patient had several episodes of fever between 38° and 39°C. In the second hospitalization, haemoculture revealed a Staphylococcus aureus infection, which was treated by antibiotics according to guidelines (Vancomycin 30 mg/kg/day in 2 doses and Imipenem 500 mg/6 hourly, the planned duration of therapy was 6 weeks). Preoperative transthoracic (TTE) and transoesophageal (TEE) echocardiography showed severe aortic insufficiency and small vegetation on the leaflets, severe mitral valve insufficiency, mild tricuspid insufficiency, and severe pulmonary valve (PV) regurgitation. This examination revealed a giant ribbon-like mobile formation (33 × 31 mm) on a pulmonary valve, which protruded into the right ventricle (Figures 1 A–C). The left ventricle ejection fraction was 45%, and end-diastolic and end-systolic diameters were 65 mm and 50 mm, respectively. The coronary angiogram was normal. Due to the high risk of an embolic event and significant ongoing haemodynamic disturbances, the heart team indicated surgical treatment. The predicted EuroSCORE II was 9.60.
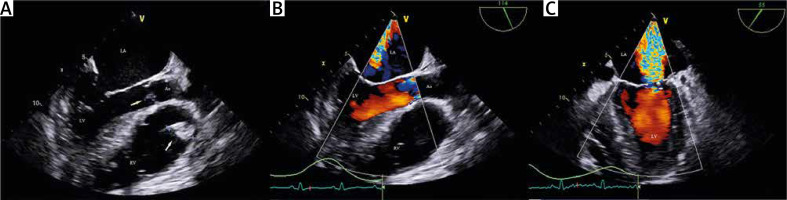
Figure 1
Transesophageal echocardiography examination: A – TEE revealed small vegetation on the aortic valve (yellow arrow) and more extensive vegetation on the pulmonary valve with protrusion into the RV. B – TEE colour Doppler examination revealed severe aortic valve regurgitation. C – TEE colour Doppler examination revealed severe mitral valve regurgitation
LA – left atrium, LV – left ventricle, RV – right ventricle, Ao – aorta.
A surgical procedure was performed through median sternotomy. Cardiopulmonary bypass was initiated using central aortic and bicaval venous cannulation. The patient was cooled down to 30°C. After cross-clamping, an antegrade cold blood cardioplegic solution was administered. Left atriotomy was made when the posterior leaflet prolapse due to primary chord rupture was revealed. The infective process damaged the free edge of the anterior leaflet, so the mitral valve was replaced with 29-mm Carbomedics mechanical valve. Subsequently, the ascending aorta was opened transversely. Destruction of the left coronary cusp was detected (Figure 2 A). Consequently, the aortic valve was excised and replaced by ST Jude Regent 21 mm. After the closure of the left atrium and aortotomy, the right atrium (RA) was opened. The septal leaflet of the tricuspid valve had shifted to the side and giant pulmonary valve vegetation was detected in the right ventricle (Figure 2 B). The pulmonary trunk (PT) and right ventricular outflow tract (RVOT) were longitudinally opened, and the valve and vegetation were excised. A 27-mm Epic Supravalve was implanted. RVOT and PT were reconstructed using a bovine pericardial patch. Vegetation was detected on the posterior cusp of the tricuspid valve, and we decided to perform resection and bicuspidization of the valve with annuloplasty by the De Vega technique. Weaning from CPB was successful with a low dose of inotropes. The duration of the cross-clamp and cardiopulmonary bypass times were 144 and 228 min, respectively. Intraoperative TEE confirmed satisfactory functioning of the aortic, pulmonary, and mitral prosthesis with trivial tricuspid regurgitation. Intraoperatively collected tissue samples remained sterile during a microbiological examination. The early postoperative course was complicated with excessive drainage and consequent revision of haemostasis. The preoperative antibiotic therapy was continued after surgery for 6 weeks. The postoperative recovery was prolonged due to the complexity of the operative treatment. The patient was discharged from our institute after 24 days and sent to the general hospital to complete his antibiotic therapy.
Figure 2
Intraoperative view: A – Surgical view on the aortic valve (black arrow) revealed destructed left coronary leaflet (white asterisk) by endocarditis process. B – Surgical view through the RA on the pulmonary valve vegetation
RA – right atrium, RCC – right coronary cusp, NCC – non-coronary cusp, LCC – left coronary cusp, TV – tricuspid valve.

Transoesophageal echocardiography performed 3 months after surgery revealed the left ventricle ejection fraction to be 50%, the end-diastolic diameter 60 mm, the end-systolic diameter 45 mm, and normal function of the implanted and reconstructed valves.
Three years after surgery, an echocardiography examination revealed normal function of the implanted prosthesis (Figure 3).
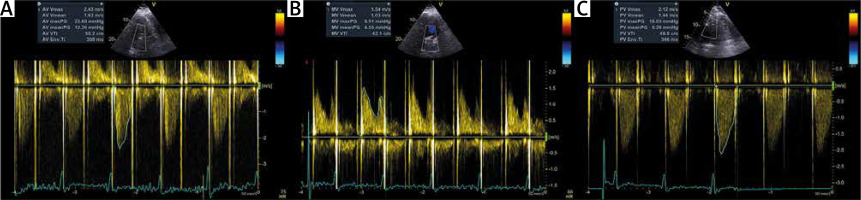
Figure 3
Tree years follow-up transthoracic echocardiography examination: A – The aortic valve prosthesis parameters. B – The mitral valve prosthesis parameters. C – The pulmonary valve prosthesis parameters
Infective endocarditis usually affects a single valve; multiple valve involvement is extremely rare. Predisposing risk factors are structural heart disease, the presence of a prosthetic valve or cardiac device, intravenous (IV) drug use, immunosuppression, or recent invasive procedures. The mortality rate is higher in patients with 2 or more affected valves than those with single valve endocarditis (between 26 and 40%). The most common aetiological micro-organism of native multivalvular endocarditis is Staphylococcus aureus (43%), and the second most common is Streptococcus viridans (36%) [2, 3]. The fundamental principles of treating infective endocarditis (IE) are microbial eradication by antimicrobial drugs, surgical excision of infected tissue, and draining abscesses. Empirical antibiotic therapy is the first line of treatment, and the choice of antibiotics is based on the clinical circumstances and suspected source of infection. According to experimental and clinical studies, bactericide drugs are more effective in treating IE than bacteriostatic drugs. Synergy, combining 2 or more antibacterial drugs, is used to shorten therapy duration and improve efficiency. The most common duration of antibiotic therapy is between 2 and 6 weeks, depending on the type of IE (prosthetic or native valve), microorganisms, and the combination of antibacterial drugs. Congestive heart failure (64%), renal failure, paravalvular leak, or fistula, as well as high risk of embolic events, are the most frequent complications of infective endocarditis [4]. In these patients, emergent (within 24 h, when pulmonary oedema and cardiogenic shock exist) or urgent (within a few days, < 7 days, in patients with HF diagnosis) surgical treatment should be considered [3, 4]. About half of the patients with IE require surgical intervention due to the mentioned complications. Although surgery in the active phase of the disease is associated with significant risk, in some cases it is a reasonable strategy to prevent adverse events and decrease the mortality rate. HF is the most common complication of IE, observed in 42–60% of patients, usually when the infection affects the aortic valve leaflets. Moderate to severe HF is a significant predictor of hospital and mid-term mortality. According to guidelines, the presence of HF is an indication for early surgical intervention, even in patients with cardiogenic shock [4]. Multiple-valve IE is frequently associated with vegetations and periannular abscess complication. Patients with multiple-valve IE and heart failure undergo urgent surgery more often than patients with SVE, mainly because of the appearance of heart failure [5]. The literature describes several successful surgical treatments of quadricuspid valve endocarditis [6, 7]. Haranahalli et al. showed a good result in the medicament treatment of a patient with quadruple-valve endocarditis [8]. The type of treatment (surgical or conservative) should be decided by the heart team, considering the haemodynamic status and response to medical management. In our case, the surgical treatment was indicated by congestive heart failure (caused by significant valve insufficiency), increased risk of embolism (due extensive vegetation on the pulmonary valve), and lack of adequate response to medical therapy.
Quadruple-valve surgery is a technically demanding but feasible procedure. Despite aggressive medical treatment, sometimes it is the only option for patients with congestive heart failure without clinical improvement. A multidisciplinary approach is necessary to avoid adverse outcomes and to provide an uneventful recovery with an excellent long-term prognosis.






