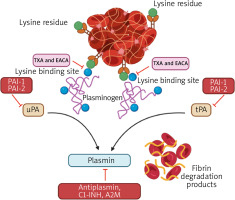
In pediatric cardiac surgery, the use of antifibrinolytic agents, specifically tranexamic acid (TXA) and epsilon-aminocaproic acid (EACA), represents a critical development in improving surgical outcomes by minimizing perioperative and postoperative blood loss and the need for blood transfusions [1]. This progress is especially notable considering the increased dangers linked to blood transfusions in young populations, such as the spread of infections and the development of sensitivities to different blood type antigens. Several studies have examined the relative effectiveness of TXA and EACA in order to improve ways of conserving blood while ensuring patient safety [2, 3]. By suppressing fibrinolysis, these medications contribute to the preservation of the structural stability of blood clots formed during surgery, as illustrated in Figure 1. As a result, they effectively reduce bleeding and minimize the potential hazards associated with blood transfusion issues. Hence, we have resolved to evaluate the efficacy and adverse effects of TXA in contrast to EACA.
Figure 1
Schematic diagram of the main mechanisms of the fibrinolytic system and the target site of tranexamic acid (TXA) and epsilon-aminocaproic acid (EACA)
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines [4]. We searched the electronic data-bases Medline, Embase, and Central from inception to March 21, 2024, for studies reporting the effectiveness and safety of tranexamic acid and epsilon aminocaproic acid in pediatric heart surgery. The literature search utilized specific keywords such as “tranexamic acid” OR “TXA” AND “epsilon-aminocaproic acid” OR “EACA” OR “6-aminocaproic acid “ AND “cardiac surgery” OR “heart surgery” IR “cardiac operation” OR “heart operation” OR “thoracic surgery” AND “child” OR “children” OR “pediatric patients” OR “newborn” OR “neonatal” OR “baby” OR “neonate” OR “neonates” OR “infant” OR “infants” OR “pediatrics”. Additionally, we manually searched the reference lists of included studies to identify additional eligible studies. We employed a random-effects meta-analysis due to the anticipated heterogeneity. Statistical analyses were performed using Review Manager (version 5.4) and Stata (version 18). The analyses were two-tailed, with statistical significance set at p < 0.05 (Table I).
Table I
Pooled analysis of outcomes of interest among tranexamic acid and epsilon aminocaproic acid
Our initial search yielded 115 publications. After the removal of duplicates (n = 61), 21 were excluded after screening titles and abstracts, leaving 33 studies for the full-text review. Manual reference list checks did not identify any additional relevant studies. After full text evaluation, a further 30 studies were excluded due to a lack of sufficient data, including no comparator group. Finally, we included 3 studies encompassing a total of 3487 participants in this review [3, 5, 6].
For the overall patient group, in-hospital mortality was observed in 26 out of 1254 (2.1%) patients for TXA compared to 61 out of 1598 (3.8%) for EACA, indicating a lower risk associated with TXA use with a p-value of 0.008. Incidents of bleeding that necessitated surgical intervention were recorded in 29 out of 1254 (2.3%) patients on TXA and 48 out of 1598 (3.0%) on EACA, showing no significant difference between the two treatments with a p-value of 0.40. Renal failure requiring dialysis was less frequent in the TXA group, with 11 occurrences out of 1304 (0.8%), versus 28 out of 1648 (1.7%) in the EACA group, showing a statistically significant reduction in risk with a p-value of 0.04. Neurologic deficits were reported in 36 out of 1304 (2.8%) patients treated with TXA and 28 out of 1648 (1.7%) with EACA, without a statistically significant difference, reflected by a p-value of 0.06. Within the neonatal subgroup, the outcomes mirrored the overall trends, with TXA typically showing a lower risk profile compared to EACA. These findings highlight the differential efficacy and safety of TXA and EACA in reducing complications in pediatric cardiac surgery, emphasizing the critical role of antifibrinolytic agents in improving postoperative outcomes.
The relative efficacy of TXA and EACA in pediatric cardiac surgery has received considerable interest, mainly because of their ability to decrease perioperative blood loss and the need for transfusions. The objective of our systematic review and meta-analysis was to evaluate the effects of TXA and EACA on surgical outcomes, specifically focusing on in-hospital mortality and renal function, as well as other comorbidities. The results of our analysis, combined with the findings of Chauhan et al. [3] and Martin et al. [6], indicate a complex situation where both TXA and EACA are successful in reducing postoperative blood loss and the need for blood transfusions. Nevertheless, our investigation revealed a significant disparity in the rates of death during hospitalization and renal problems between the two substances. Specifically, EACA was found to be linked to a slightly higher mortality rate and an elevated likelihood of renal injury.
This discrepancy in results emphasizes the importance of carefully selecting antifibrinolytic medication, taking into account the advantages of lowering blood loss while considering the potential dangers of negative side effects. A comprehensive understanding of the patient’s unique situation, including pre-existing risk factors for renal dysfunction and the overall risk profile for mortality associated with their heart illness, should guide the decision-making process. Furthermore, our findings underscore the importance of continuous monitoring and evaluation of kidney function in children undergoing heart surgery, especially when EACA serves as the antifibrinolytic medication. When deciding between TXA and EACA, it is important to carefully evaluate the patient’s specific clinical situation. This involves comparing the effectiveness of each agent in minimizing surgical bleeding with their individual risks of mortality and renal injury.
Our systematic review and meta-analysis elucidate the comparative effectiveness and safety of tranexamic acid and epsilon-aminocaproic acid in pediatric cardiac surgery, revealing no significant difference in their ability to reduce surgical bleeding and the need for transfusions. However, a notable finding was the slightly higher mortality rate and increased risk of renal injury associated with EACA, as opposed to TXA. These results suggest that while both TXA and EACA are valuable in minimizing perioperative and postoperative complications, their use must be carefully tailored to the patient’s specific risk factors and clinical needs. In light of the observed differences in safety outcomes, particularly concerning mortality and renal function, clinicians should exercise heightened vigilance when selecting an antifibrinolytic agent, prioritizing both the efficacy and safety profiles of these medications. Future research should focus on further clarifying the risk-benefit ratio of TXA and EACA in pediatric cardiac surgery, aiming to optimize antifibrinolytic therapy for improved patient outcomes while minimizing adverse effects.
This analysis underscores the critical role of antifibrinolytic agents in minimizing surgical and postoperative complications, emphasizing the nuanced differences in their effectiveness and safety profiles. The findings provide evidence-based insights that can guide clinical decision-making in pediatric cardiac surgery, contributing to improved patient outcomes and reduced healthcare burdens associated with blood transfusions and postoperative complications.






