Introduction
Early melanoma detection is a crucial factor that affects further patient prognosis [1]. However, during the COVID-19 pandemic healthcare systems around the world were made to redirect their resources towards the most urgent conditions. Even though oncological diseases in Poland, including cutaneous melanoma (CM), were uninterruptedly considered a priority, an actual, cumulative effectiveness of introduced solutions remains unknown. Previous research performed in other centres from different countries presented inconclusive results [2–5].
Aim
In this study, we sought to assess whether the coronavirus pandemic affected the diagnosis of melanoma at our medical centre.
Material and methods
We conducted a retrospective single-centre study, which compared cases of melanoma diagnosed in the Dermatology Department in Gdansk in two corresponding periods: from March 2018 to June 2019 – a pre-COVID period (pre-CP), and from March 2020 to June 2021― the COVID period (CP). The time span was selected specifically to avoid any bias, as the diagnostic and therapeutic approach during those two periods were comparable in terms of personnel, available equipment, and place of treatment. The only relevant differences were organisational modifications introduced as a response to the COVID-19 outbreak.
The evaluated variables included those concerning the patient in general (gender, age) and those describing the lesion specifically: anatomical location, tumour size and morphology, presence of ulceration, Breslow thickness and pT stage. P-values < 0.05 were considered statistically significant. The analysis included 66 histologically confirmed cases of melanoma in adults (≥ 18 years) in the pre-CP and 52 in the CP. It is worth mentioning that due to a relatively small number of enrolled patients, a two-sided Fisher exact test was performed when comparing patient categories and a two-sided Wilcoxon Rank-Sum test was used to compare numerical data. Some data could be only analysed by a percentage change (%Δ), for the same reason.
Results
A total of 118 cases of histologically confirmed CM were included in the study. The demographic structure and tumour characteristics are shown in Table 1.
Table 1
Comparison of the examined clinical and histopathological variables of melanoma in the pre-COVID period (pre-CP) and COVID period (CP)
We noted a 21.2% reduction in the number of all melanoma cases diagnosed during the CP. We have found no significant differences between the analysed time periods regarding patients’ age or sex. There was no significant change in the presence of ulceration, Breslow thickness, tumour size and mitotic rate. However, there was a tendency for melanomas diagnosed during the CP to be less frequently located on the trunk (40.91% pre-CP vs. 26.92% CP), while the incidence of CM in other anatomical locations was marginally affected (head: 19.70% pre-CP vs. 26.92% CP, limbs: 39.39% pre-CP vs. 46.15% CP) (Table 1).
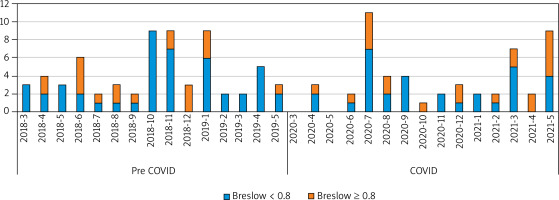
We also performed an analysis of the pT parameter distribution. We separated early melanomas (pTis + pT1a) from remaining stages as the treatment of choice in those cases is much less challenging and is limited to wide resection, without the need of sentinel lymph node biopsy. The results indicate that there was a significant drop in early melanomas in the CP (p = 0.0011) (Figure 1).
Discussion
The data suggest that the COVID-19 pandemic influenced melanoma management mainly at the stage of the diagnostic process preceding patients’ referral. There was a considerable reduction in the overall number of melanomas detected in our study (21.2%). A similar trend was observed in other countries – a lower incidence was reported by Lallas et al. [2] in Greece (36.4%) and Koch et al. [3] in Chile (31.2%).
Secondly, we noted that during the CP there was a tendency towards more advanced melanoma cases. The same trend was also noticed by Koch et al. [3] in Chile and Shannon et al. [4] in the United States.
Similarly to comparable studies, we found no significant trends concerning age or sex of the patients. The only difference on this matter was presented by Lallas et al. who found the population during lockdown to be younger than predicted [2].
The occurrence of CM diagnosed on the trunk decreased by 13.99% of the total count, while the number of lesions located elsewhere remained similar. This could reflect the fact that during the pandemic some social activities that involve body trunk exposure (swimming pool/gym attendance, warm-climate tourism) were limited or prohibited and the patients were less likely to be warned about suspicious skin lesions beyond their vision range. A similar mechanism of poor self-detection of melanomas appearing on non-easily visible locations was described by Avilés-Izquierdo et al. in 2016 before and irrespectively of the pandemic [6]. The second possible explanation was the fact that some of the melanomas not accessible during self-examination were not detected as the patients postponed dermatological follow-up visits due to fear of the COVID-19 infection. Other authors did not analyse the anatomical location of CM during the pandemic [2–5].
Taking into account that the procedures concerning the management of CM were not modified in our department during the pandemic, patient-dependent factors discussed above must have been crucial. The study’s limitations are a relatively low number of patients and a single institution structure. Further research is needed to determine the influence of the COVID-19 pandemic on melanoma outcomes.