Clinical pharmacology has changed many clinical systems, including anaesthesia delivery in both the hospital and ambulatory surgery settings. Ambulatory surgery centres, also known as outpatient care centres, are facilities that provide same-day healthcare services to patients, which are cost-effective and convenient. These facilities can offer surgical care, intervention, and diagnostic and preventative procedures (Figure 1). Ambulatory surgery centres may choose to perform procedures in one specific specialty or instead offer a broad range of services. These facilities are revolutionary because they provide an alternative to hospital-based outpatient services and generally provide favourable patient outcomes. Ambulatory surgery centres have increased across the USA, related to the expansion of minimally invasive and noninvasive procedures and advances in anaesthesia and analgesia with improved drugs with better duration, quicker recovery, and fewer side effects.
Enhanced recovery after surgery (ERAS) was established to improve patient care and increase the number of available ambulatory surgery centres [1]. ERAS was created to enhance perioperative care, improve recovery through evidence-based research, and to implement evidence-based practice. ERAS can also be referred to as a “process” that involves every aspect of surgery that can affect patient recovery including preoperative, intraoperative and postoperative care. ERAS implements enhanced patient care and recovery by focusing on preoperative patient nutrition, avoidance of prolonged patient fasting, implementing multimodal analgesia, regional anaesthesia, decreasing opioid utilisation, and encouraging patient resumption of diet and mobilisation as early as possible during the perioperative period. There are ERAS guidelines available for nearly every specialty in healthcare, and ambulatory surgery is no exception. ERAS guidelines’ goal to reduce patient recovery time and improve patient outcomes align with the mission of ambulatory surgery centres. By implementing ERAS protocols, ambulatory surgery centres can provide cheaper services while maintaining the efficiency of their centre.
HISTORY AND BACKGROUND OF ERAS IN AMBULATORY SURGERY
The concept of ERAS was first established and advocated by the Danish surgeon Henrik Kehlet [2]. By focusing on multimodal interventions to limit surgical stress, Kehlet aimed to reduce unfavourable sequelae, shorten the length of hospital stay, reduce costs, and improve patient recovery. Kehlet’s work demonstrated that with “fast track” surgery, patients who underwent open sigmoid resections were ready to be discharged only two days after surgery [3]. At the time, postoperative care greatly varied within Europe, and recovery times for an open sigmoid resection could last between five and 10 days [3, 4].
As ERAS interventions continued to be developed and more uniform approaches were taken to optimise patient recovery, studies revealed the effectiveness of changes in perioperative management. A retrospective cohort study of over 900 patients who underwent major colorectal cancer surgery determined that in patients with higher adherence to ERAS interventions, the risk of five-year cancer mortality was lowered by more than 40% compared to those with lower compliance [5]. Studies over the following decade demonstrated significantly improved patient outcomes with more structured guidelines and prompted the formation of the ERAS Society in Sweden in 2010 [4]. The goal of the ERAS Society is to improve patient recovery through implementation of evidence-based practice, and their guidelines continue to change to meet their goal.
ERAS encompasses all care regarding a procedure, including preoperative counseling, intraoperative monitoring, and postoperative follow-up [6]. New guidelines for perioperative care focus on reducing multiple physiological stressors of surgery, including hormonal, neurological, and metabolic disturbances that alter organ function. Physical symptoms of these disturbances include nausea, vomiting, and pain, which are among the most common causes of delayed discharge following ambulatory surgery [7, 8].
Because implementing ERAS produced significant improvements in patients who underwent colorectal surgery, ERAS guidelines have been applied to many other specialties, including breast reconstruction, liver surgery, pancreaticoduodenectomy, head and neck surgery, gynaecology, urology, and anaesthesia. Therefore, any ambulatory surgery centre that performs these types of services can and subsequently does utilise ERAS. Furthermore, since the purpose of ambulatory surgery centres is to provide reliable patient care with a swift turnaround, ERAS guidelines provide the perfect framework to make ambulatory surgery centres even more efficient at reducing costs to both the patient and the centre.
GUIDELINES IN AMBULATORY SURGERY WITH A CLINICAL PHARMACOLOGY FOCUS
Preoperative ERAS
The goal of preoperative ERAS is to physiologically and psychologically prepare the patient for surgery and recovery. This section focuses on ERAS protocols implemented before surgery with the aim of constructing the framework for enhanced recovery. This includes: patient education, preoperative medications (post-operative nausea and vomiting [PONV], infection prevention, thrombus prophyla-xis), fluid therapy, nutrition, carbohydrate loading, mechanical bowel preparation, and minimising fasting. ERAS protocols originating in the preoperative period will improve patient outcomes throughout their recovery.
Preoperative patient education
The main goals of preoperative education are to inform the patient of what to expect for surgery, to establish achievable goals for managing postoperative pain and to identify additional patient needs following surgery. Preoperative education includes communicating with the patient about what to expect in terms of pain and recovery time and instruction on procedural preparation and follow-up [9]. Taking this step to educate patients and understand their expectations surrounding surgery has been associated with significantly less stress and anxiety and increased levels of confidence regarding surgery and surgical outcomes. It is vital to understand patient expectations about postoperative pain to ensure an understanding that, regardless of the approach to postoperative analgesia, some discomfort is inevitable [10]. A major goal of ERAS is to reduce preoperative use of opioids and anxiolytics. Arguments exist that preoperative anxiolytics can be avoided in some patients, with proper preoperative counseling and reassurance [11].
Preoperative patient medication
A goal of ERAS protocols is to reduce postoperative complications with prophylaxis of nausea and vomiting, infection, and thromboembolism in appropriate patient populations. Furthermore, ERAS utilises a multimodal approach to decrease anxiolytics and opioids preoperatively. Preoperative screening to stratify the patient’s risk for PONV is important. Risk factors include history of PONV or motion sickness, female gender, being a non-smoker and the use of opioids following surgery. Once the patient’s risk is ascertained, the appropriate antiemetic combination can be ordered prior to surgery and available in the patient’s chart for more timely use. These antiemetic medications can include those affecting serotonergic, dopaminergic, or cholinergic receptors [12]. Some non-pharmacological recommendations for minimising or preventing PONV include maintaining adequate hydration, preoperative carbohydrate loading, and reducing preoperative fasting [12], as well as the use of a total intravenous anaesthetic and avoidance of inhaled volatile anaesthetics such as nitrous oxide [12].
For certain high-risk procedures and for patients determined to be at higher risk of infection, prophylaxis with antibiotics is recommended. For example, the Society of Thoracic Surgeons recommends prophylactic treatment with a beta-lactam antibiotic 30 minutes prior to and two days after cardiac surgery. Other factors such as known organisms and resistance patterns, patient allergies, and type and duration of procedure must be considered prior to choosing presurgical infection prophylaxis [13]. The National Nosocomial Infections Surveillance score system is a widely accepted system to stratify a patient’s risk of postoperative infection. Using the system’s criteria, a determined score of > 1 requires consideration of prophylactic antibiotic administration [14, 15].
The ERAS protocol recommends prophylactic anticoagulation for patients undergoing surgery with increased risk of venous thromboembolism, following clearance of bleeding risk factors [16]. Pharmacological interventions include the use of unfractionated heparin or low-molecular-weight heparins prior to surgery. Some non-pharmacological options include intermittent pneumatic compression devices and simple compression stockings. The American College of Chest Physicians has published guidelines and standards for perioperative antithrombotic therapy, which include assessing the patient up to one week prior to surgery to screen and discuss use and management of anticoagulants, and to provide a calendar for the timing and discontinuation of therapies and laboratory studies, international normalised ratio (INR) studies prior to surgery, and postoperative haemostasis assessments [17].
Preoperative fluid therapy
One major complication that prolongs hospital stays following surgery is dehydration. ERAS recommends the use of goal-directed fluid therapy to present patients to the operating room in a euvolemic condition to minimise complications relating to fluid volume. Both hypovolaemia and hypervolaemia are associated with postoperative morbidity [18]. Hypovolaemia leads to vessel constriction, which ultimately affects organ function by diminishing oxygen delivery. Hypervolaemia can cause local inflammation and oedema, which can delay healing and increase infection risk [19]. Traditionally, urine output was the gold standard for assessing volume status. It has since been determined that this is not a sensitive indicator due to other factors, including prostatic enlargement and flow obstruction, which can alter urine volume [20]. Some noninvasive techniques for determining volume status in a preoperative patient include heart rate, blood pressure, and laboratory electrolyte studies. More invasive techniques such as pulmonary artery catheterisation or arterial waveform-based analysis can also be used to decide whether a patient needs fluid therapy [18]. Use of goal-directed fluid therapy leads to less infection and organ dysfunction and fewer transfusions required postoperatively [21].
Preoperative nutrition
It is important to assess the nutritional status of each patient preoperatively, because malnutrition is a positive predictor of postoperative complications. Malnutrition prior to surgery is associated with increased readmission rates, longer hospital stays and complications such as delayed wound healing and infection [22]. Screening questionnaires should be used for assessment of nutritional status, and consultation of a dietician is recommended if malnutrition is suspected. If a patient can enter surgery in a metabolically fed state, retention of lean muscle mass and avoidance of extreme protein loss are possible and conducive to better recovery overall [23].
Carbohydrate loading
The ERAS protocol recommends carbohydrate loading with a clear liquid 2–3 hours prior to surgery in appropriate patient populations. Carbohydrate loading has been linked to improvements in insulin sensitivity, as well as less reported hunger and thirst prior to surgery. Consumption of carbohydrates prior to surgery also protects from some of the catabolic effects associated with fasting and reduces infections, duration of hospital stay, and complications overall [24, 25]. One study associated preoperative carbohydrate treatment with decreased ER visits and hospital readmissions due to pain [26]. These regulations should be used with caution in patients with diabetes and gastric motility disorders that slow gastric emptying and increase the risk of aspiration during surgery [27].
Mechanical bowel preparation
The goal of preoperative mechanical bowel preparation (MBP) is to reduce the solid faecal contents and bacterial load of the colon. Liquefaction of solid faeces may, however, cause increased risk for intraoperative spillage and contribute to presurgical dehydration [28]. Some other complications and disadvantages of MBP include increased length of hospital stay, more reported abdominal pain, fluid and electrolyte imbalances and risk of infection [29]. The ERAS protocol suggests limitation or avoidance of bowel prep if possible, but some recent evidence conflicts with this recommendation, stating that some of these risks can be curbed with treatment with prophylactic antibiotics in combination with MBP [30].
Avoidance of fasting
ERAS programs have changed the guidelines for fasting prior to elective surgery. Due to a lack of evidence supporting additional safety from long periods of fasting, as well as evidence that the prolonged fast could actually increase the catabolic stress responses following surgery, causing hyperglycaemia and insulin resistance, it is now acceptable to continue solid food up to six hours and clear liquids up to two hours before induction [12, 31]. Reduced fasting periods improve patient outcomes and satisfaction due to less thirst and hunger sensation and decreased risk for dehydration [21]. These regulations should be approached more cautiously for uncontrolled diabetics, morbidly obese patients, or those with gastric motility issues [32].
Intraoperative ERAS
Intraoperative ERAS protocols aim to minimise surgical stress on the patient. This section focuses on ERAS protocols implemented during surgery, including opioid-sparing analgesia, multimodal analgesia, regional anaesthesia, avoiding drains, avoiding salt and water overload, and maintaining normothermia. It is important to continue other ERAS protocol aspects during surgery, such as analgesia and prevention of PONV. Implementing ERAS interventions in surgery decreases postoperative morbidity and aids recovery.
Opioid-sparing analgesia
Due to the current opioid epidemic, ERAS recommendations are attempting to reduce patient dependence on opioids postoperatively. Opiates are used intraoperatively for analgesia, but ERAS guidelines state that short-acting or ultra-short-acting opioids are preferred to long-acting opioids if possible. Short-acting opiates, such as fentanyl, do not cause as much respiratory depression as longer acting opiates do, and are therefore preferred [33].
Postoperative use of opioids is strongly recommended against by ERAS, and reducing opioid use is the motive behind the new multimodal analgesic approach. With this approach there are hopes to use combinations of pharmacological therapies to achieve the same analgesic effects of opioids without the side effects. Side effects include constipation, urticaria, urinary retention, nausea, bowel ileus, respiratory depression, hypotension, confusion, tolerance and dependence. If a patient is still experiencing pain despite the multimodal analgesia, then ERAS recommends self-administered opioids as the patient needs them. This will eliminate creating a standard dose for patients, keeping the treatment personalised to prevent overuse [33].
Multimodal analgesia
Clinical pharmacology has aided greatly in the concept of multimodal analgesia. In essence, there are additive or synergistic effects from drugs, typically mediating or modulating different pathways with improved clinical outcomes. Pain, which has been coined the “fifth vital sign”, has proven to be an important factor in surgical outcomes and patient recovery. With the goal of improving patient outcomes while reducing the psychological stress of surgery, relieving pain became a key focus in the ERAS guidelines [9]. The idea of using a multimodal analgesia model is meant to incorporate multiple pharmacological agents to decrease the use of opiates, avoiding their use whenever possible [34].
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a well-known drug class with both anti-inflammatory and analgesic properties. NSAIDs mediate their effects through inhibition of the enzymes cyclooxygenase (COX)-1 and COX-2, decreasing the synthesis of prostaglandins. In a systematic review, it was found that patients with acute pain greatly benefited from taking NSAIDs compared to a placebo. The study also showed that NSAIDs were more effective for treating acute pain than intramuscular morphine. Side effects associated with NSAIDs include increased risk for stomach ulcers and bleeding [35]. Cases have been reported of increased risk for anastomotic complications in patients undergoing colorectal resections and this should be taken into consideration when using NSAIDs [36]. ERAS recommendations promote the use of NSAIDs in this opioid-sparing model, with precaution taken in colorectal surgery patients and others that have contraindications [37].
Another class of drugs that have been explored are the N-methyl D-aspartate (NMDA) receptor antagonists, which exhibit nociceptive effects by inhibiting the release of the excitatory neurotransmitter glutamate. These drugs include ketamine, memantine and magnesium sulphate. A recent study that demonstrated that when given ketamine intraoperatively, patients used smaller amounts of self-administered opioids in the first 24 post-operative hours [38]. Although this does fit the goal of ERAS’s effort to reduce opioid use, there have not been enough investigations on the use of ketamine intraoperatively, so at this time it is not currently in the recommendations [37].
Gabapentin and pregabalin have also been included in the multimodal approach of postoperative analgesia. Although some studies have found that these drugs can reduce opioid use and pain postoperatively, there has not been a good consensus on how to use these drugs safely in combination with others [39]. Related to the current inconclusive data, gabapentin and pregabalin have not yet been added to the ERAS guidelines, but continue to be investigated [37].
Regional anaesthesia
The intraoperative use of IV local anaesthetics has become a new area of research. Recent investigation of the use of IV lidocaine infusion intraoperatively has shown great analgesic effects, particularly in abdominal procedures. These effects are limited because similar results were not found in orthopaedic surgery, cardiothoracic surgery, or tonsillectomy [40]. A meta-analysis found that patients who received IV lidocaine had fewer post-operative complications, shorter lengths of stay in the hospital, and less postoperative opioid consumption [41]. The addition of using local anaesthetics can now be found in several of the ERAS guidelines.
Local anaesthetic infusion can also be performed via the midthoracic epidural route in patients undergoing colorectal surgery. ERAS guidelines call for the infusion two days postoperatively for the best outcome. It has been shown that this provides better analgesia in this patient population than in patients administered opioids [42].
No drains
Historically, drain placement following rectal or colonic surgery was the mainstay of care. Questions were raised after a systematic review showed that there was no benefit from prophylactically placing a drain in colorectal surgery for the prevention of anastomotic leakage [43]. After several more analyses provided similar results, ERAS concluded that drains should not be placed in most situations.
A study evaluated the effectiveness of ERAS guidelines in gynaecology oncology surgery, which included the elimination of drain usage. The results showed that the ERAS group returned to bowel function earlier, had shorter hospital stays, and experienced satisfaction with their treatment compared to the control group [44].
Avoidance of salt and water overload
Fluid management in ERAS is monitored throughout the preoperative, intraoperative, and postoperative stages. Intraoperative fluid balance aims to maintain euvolaemia while avoiding salt and water overload. Maintenance fluid therapy can be achieved by administering crystalloid solution with the purpose of trying to maintain the patient’s preoperative body weight. For most patients, this is sufficient to keep them euvolaemic [21]. For more serious procedures, the fluid challenge may be implemented to ensure that the patient is maintaining an adequate fluid level. This should be done when it is suspected that the patient is volume deficient. Heart rate and mean arterial pressure are often used to evaluate the patient’s volume status, but this is not always completely accurate [21].
Maintenance of normothermia
Some methods of maintaining body warmth include forced air warming, IV fluid warming, electric blankets, irrigation fluid warming, warming of insufflation gases, circulating water mattresses and warming of anaesthetic gases. Reducing hypothermia intraoperatively can decrease post-operative shivering and cardiac events [21].
ERAS in the postoperative period
The goal of ERAS programs in the postoperative period is to decrease morbidity and return the patient to a fully functional status as soon as possible. This section focuses on ERAS protocols implemented in the postoperative period. This includes: stimulation of gut motility, early feeding and postoperative nutrition, prevention of postoperative ileus, avoiding NG tubes, early mobilisation, early catheter removal, and how to audit ERAS compliance and outcomes. It is important to continue other ERAS protocol aspects in the postoperative period such as analgesia and electrolyte and fluid balance, to decrease morbidity and length of stay. The postoperative ERAS protocols work together synergistically to improve the recovery of the patient – no intervention is truly separate from the others.
Early feeding and postoperative nutrition
Preoperative fasting is part of anaesthesia practice guidelines to reduce perioperative pulmonary aspiration [32]. ERAS guidelines recommend decreased preoperative fasting as well as carbohydrate loading before surgery, as described above. These protocols help patients remain in a fed state for a longer duration of physiologically taxing surgery. However, the patients still fast for several hours and will enter a catabolic state in surgery or early in recovery [45]. During catabolic states, patients become insulin resistant and begin to lose nitrogen and protein reserves [46].
To decrease catabolic stress, ERAS guidelines encourage feeding as soon as orally tolerated by the patient. Early feeding increases gut motility, which decreases the risk of postoperative ileus. Most patients can drink fluids immediately and eat normal hospital meals with a daily caloric intake of 1200–2000 as soon as they can tolerate oral intake [47]. Patients with surgery-specific nutritional or supplemental needs, such as increased iron and vitamin B12 after some bariatric procedures, can begin their supplementation immediately with their oral diet [48]. The postoperative diet should include the calories and macronutrients required by the particular patient. Maintaining glycaemic control in patients with diabetes is key in the postoperative time period because insulin resistance often increases in surgery. Evidence shows that ERAS early feeding protocols actually decrease insulin resistance compared to “nil by mouth” in the postoperative period [30, 47, 48].
The main risk of early feeding is pulmonary aspiration, requiring the patient to go back under anaesthesia [16]. Therefore, early feeding should be carefully balanced with complications in high risk patients in the immediate post-operative period.
Prevention of postoperative ileus and stimulation of gastrointestinal motility
Gastrointestinal (GI) dysfunction is a common neurogenic sequela of the sympathetic stress response. Nociceptive afferents and sympathetic efferents contribute to the post-operative inhibition of organised propulsive activity. Postoperative bowel dysfunction is most common in, but not limited to, colorectal or abdominal surgery. The increased sympathetic tone after surgery and trauma can lead to paralytic and edematous enteric tract structures [46, 49]. There is little formally defined distinction between “pathologic ileus” and expected short-term post-anaesthesia GI dysmotility. Here, ileus will be defined as severe bowel dysmotility that is characterised by nausea, vomiting, abdominal pain and distension, and delayed passage of flatus/stool that slows recovery and leads to further complications. This is in contrast to temporary dysmotility following anaesthesia that resolves within hours and does not lead to further complications [50].
Postoperative ileus has many negative consequences including abdominal pain, decreased appetite leading to a prolonged catabolic state, and mucosal barrier damage leading to bacterial translocation and increased physiologic stress [2, 49]. IV and epidural opioids used for intra- and postoperative analgesia and sedation are associated with ileus and a longer period of decreased gut motility after surgery [51]. ERAS protocols recommend the use of opioid-sparing perioperative analgesic and sedative medications [16]. Local anaesthetic epidurals can be used instead of opioids. Local anaesthetics have the same amount of pain control during surgery but they allow a faster return of bowel function, decreasing risk of ileus [51].
Postoperative paralytic ileus risk is also increased in fluid overloaded states. Maintaining an intraoperative salt and water balance, as well as postoperative electrolyte monitoring, decreases this risk [47]. Early feeding and fluid intake stimulate peristalsis, activating vagal signals to the enteric tract while simultaneously inhibiting sympathetic tone. This early increase in gut motility prevents ileus and subsequent delays in healing [46, 50].
Avoid nasogastric tube
A postoperative nasogastric (NG) tube should not be routinely used for ERAS patients. Rather, the need should be determined case by case and only used when totally necessary. Patients who undergo postoperative NG decompression have higher levels of aspiration-related sequelae including fever, atelectasis and pneumonia. Patients with an NG tube also have a delayed return of bowel motility and function – indicated by an increased time until the first flatus or stool after surgery. Postoperative NG tubes delay first oral intake and cause patients added discomfort [46–48, 52]. If an NG tube must be placed for gastric decompression or otherwise, it should be removed before the patient is extubated to reduce aspiration risk [46].
Early mobilisation
Prolonged immobilisation after surgery slows down healing and increases time to functional recovery. Patients ideally should be mobilised within 24 hours of their surgery, which heavily relies on pain control and hydration status. Early mobilisation is associated with many physiological and psychological benefits that result in decreased hospital stay and a shorter recovery time [6, 16]. Longer immobilisation increases the length of time the patient is in a postoperative catabolic stressful state, which delays healing and creates other problems including deep venous thrombosis formation and thromboembolism, orthostatic hypotension, and pulmonary complications [2].
Early catheter removal
Unless specifically indicated, urinary catheters in ERAS patients should be removed at the end of the operation. Early catheter removal decreases the risk for urinary tract infections and decreases the amount of time the patient needs to be in a recovery bed [53]. Continued catheterisation both restricts ambulation and is uncomfortable for the awake patient – both factors increase physiological and psychological stress. The main risk consideration of early urinary catheter removal is postoperative urinary retention, especially in pelvic or abdominal surgery patients with epidural anaesthesia. There are conflicting data on the rates of urinary retention in the field of ERAS. The current data support catheter removal at the end of anaesthesia, unless otherwise indicated, and monitoring the patient with bedside bladder ultrasound if they are unable to urinate [54]. Overall, prolonged use of urinary catheters limits recovery; therefore catheters should be removed as early as safely possible in ERAS patients [44].
Audit of compliance and outcomes
A central tenant of ERAS is regular team audits of compliance and outcomes. The ERAS Society created its own online audit tool, which can be found on its website along with the ERAS protocols for various surgical subspecialties. This audit tool focuses on shorter patient recovery time, decreased complications and improved quality of care [55]. Teams providing ERAS care should meet frequently at the onset of new protocols [56]. Audits including the whole team are valued because team meetings foster cohesive attitudes that champion ERAS and lead to stronger adherence to protocols, and therefore better patient outcomes [57, 58]. Patient care teams need 70–80% compliance to ERAS protocols to see improved outcomes [56].
SUMMARY OF THE ROLE OF CLINICAL PHARMACOLOGY WITH ERAS IN PERIOPERATIVE CARE
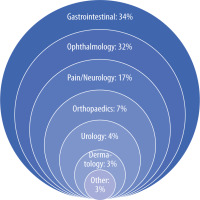
Enhanced Recovery After Surgery protocols arose out of the need to decrease physiological and psychological surgical stress. ERAS aims to reduce unfavourable sequelae, shorten the length of hospital stay, reduce costs, and improve patient recovery. Surgical subspecialties have embraced the philosophy of ERAS, creating unique protocols to meet their patients’ needs (Figure 2), highlighting interventions in the preoperative, intraoperative, and postoperative periods that reduce patient surgical stress. ERAS emphasises teamwork, necessitating frequent audits on compliance to continually improve patient outcomes.
IMPORTANCE OF OPIOID-SPARING ANALGESIA IN AMBULATORY SURGERY CENTRES
There has been a strong focus on non-opioid techniques in ERAS due to the current opioid crisis in the United States. Opioids still play an important role in intraoperative analgesia, but the focus has turned to a multimodal approach to reduce opioid use in patients overall. Multimodal analgesia does not use a singular intraoperative and postoperative medication or technique, but rather uses a combination of various pharmacological principles to provide adequate pain control while also limiting the postoperative course. Certain multimodal techniques for pain control have been incorporated into ERAS protocols, including regional blocks, non-opioid analgesia, and minimal use of opioids. Ketamine, gabapentin, dexmedetomidine, intravenous lidocaine, NSAIDs, and acetaminophen have been used in various combinations intraoperatively to decrease the need for postoperative opioids (Table 1). This concept is based on using pharmacologic synergy to maximise positive effects while minimising the side effects [59]. Ketamine has had renewed interest amongst anaesthesiologists due to the NMDA properties and pain relief capabilities. A recent systemic review demonstrated that the combination of low dose ketamine combined with opioids showed an overall decrease in the use of opioids while also having better pain control without serious side effects [60]. Gabapentin has also been used in various multimodal techniques. It inhibits presynaptic voltage-gated calcium channels in the dorsal root ganglia of the spinal cord. During surgery, these channels are active and upregulated, which can be inhibited by gabapentin. Optimal dosing and timing have not been established, but typically ERAS pathways use gabapentin and pregabalin dosing around two hours prior to any procedure [39]. Clonidine and dexmedetomidine have also been studied in the setting of pain control. Interest in dexmedetomidine in relation to anaesthesia and the sleep/wake cycle has been a hot topic in the current literature. Alpha-2 agonists can stimulate those receptors in the spinal cord and supraspinally which result in antinociceptive responses. It has been shown that clonidine and dexmedetomidine reduce opioid consumption postoperatively [61]. Lidocaine, which intravenously has typically been used as an antiarrhythmic, has gained recent traction as an adjunctive pain control medication. The blockade of sodium channels can modulate neuropathic pain. Lidocaine has analgesic and anti-inflammatory properties. Additionally, lidocaine and other local anaesthetics have been used in various regional anaesthetic techniques to help in the immediate postoperative period regarding pain control [62]. NSAIDS and acetaminophen have been used in combination with the above methods to decrease opioid consumption in the immediate post-operative period in ambulatory surgery. ERAS protocols are designed to incorporate these pain control regimens into their pathways in ambulatory surgery to increase efficiency and patient satisfaction while also controlling pain using limited opioids.
TABLE 1
Multimodal analgesia for enhanced recovery after surgery (ERAS). Adapted from [63]
TABLE 2
Benefits of ambulatory surgery centres
TABLE 3
Key issues in enhanced recovery after surgery (ERAS)
FUTURE DIRECTIONS WITH A FOCUS ON CLINICAL PHARMACOLOGY AND ANAESTHESIA
Implementation of ERAS as a standard of care is starting to gain popularity. However, ERAS is not yet a strictly enforced paradigm, and it is usually left to the discretion of the management staff at the healthcare facility whether ERAS is implemented in healthcare practice. Education of healthcare providers regarding the benefits of ERAS is probably the best way to ensure the further practice of ERAS in all healthcare facilities, and to educate healthcare providers about the benefits of ERAS there must be published peer-reviewed clinical trials that measure the effects of ERAS. To date, there are very few studies that investigate the effects of ERAS, although the studies that have been published show that ERAS is effective at improving patient outcomes. Research that focuses on evaluating the sequence of perioperative complications will be beneficial. Currently, most ERAS studies focus on patient outcomes, which, although important, have already been established. It will also be beneficial to gather data on patients after discharge to see the long-term benefits of ERAS. With regard to education, healthcare providers, as the forefront of patient care, including medical students, residents, fellows, and nurses, should be a top priority for the introduction to and implementation of ERAS. The earlier that healthcare providers can learn about the benefits of ERAS, the more likely it is to be used in clinical practice. Physicians should lead by example and ask that ERAS guidelines be used by their staff.
The development of new technology that can help to improve patient care, as well as technology that can help measure patient outcomes, will all be useful for the future of ERAS. Devices such as pneumatic leg compressors, oesophageal dopplers, and forced air warming units can foster the implementation of ERAS. Furthermore, the progression of wearable physiological monitoring devices in everyday life can be utilised to foster ERAS. These devices make it possible to monitor patient physiology continuously, which can be used for patient follow-up and for enhanced perioperative care when the patient undergoes surgery.
Many ERAS pathways are used in anaesthesia practice including the hospital and ambulatory surgery settings with a strong focus on clinical pharmacology, concentrating on preoperative, intraoperative, and postoperative outcomes. Preoperatively, the focus should be on patient counseling regarding what to expect leading up to surgery, including the day of surgery, as well as postoperative expectations. Ultimately this can reduce anxiety and confusion for the patient and family members [64]. Smoking cessation is also one of the most important health interventions that can be applied in the preoperative setting. Aggressive smoking and alcohol cessation 6–8 weeks prior to surgery can reduce postoperative morbidity by 50% [65]. Preoperative exercise can reduce the postoperative stay and risk of pulmonary complications in the postoperative setting. Overall, exercise improves inspiratory muscle strength and endurance and reduces pain and anxiety [66]. Preoperative metabolic optimisation is a technique incorporated into many ERAS protocols which includes various techniques aimed at reducing the inflammatory reactions. These techniques include carbohydrate loading, perioperative glycaemic control, preoperative enteral feeding, immune modulating nutrition, and addition of trace vitamins and minerals. Clinical application of ERAS protocols in the intraoperative setting include a focus on multimodal analgesia, fluid and salt balance, maintenance of normothermia, and avoidance of opioids if possible. These techniques have been shown to decrease patient complications when applied to the intraoperative setting [67].