Introduction
Colorectal cancer is the third most common cancer in the world, with 1.8 million new cases of colorectal cancer and more than 800,000 deaths worldwide in 2018 [1]. Colorectal cancer has significant racial differences, with gender differences having the highest incidence in African Americans, with males greater than females [1]. The 5-year survival rate for colorectal cancer is 65% in developed countries, but it is still less than 50% in low-income countries [2]. Standard treatments for colorectal cancer are surgery, radiation and chemotherapy [3]. Colorectal cancer seriously endangers human health, and it is necessary to actively explore treatment methods.
The traditional surgical treatment for resectable colorectal cancer is open surgery. With the development of laparoscopic technology, the invention of hand-assisted laparoscopy (HLA) and single-port laparoscopy (SLA), minimally invasive surgery has also been used in colorectal cancer surgery, because of its inconspicuousness and aesthetics, lower incidence of incisional hernia, and fewer wound complicatons [4, 5]. Laparoscopic surgery for colorectal cancer requires an incision for specimen extraction, and the commonly used incisions are: right lower quadrant/left lower quadrant (RLQ/LLQ), stoma site, infra-umbilical midline, periumbilical midline, Pfannenstiel, etc [6, 7]. However, the choice of specimen extraction incision is unclear for surgical treatment of colorectal cancer [8]. The Pfannenstiel incision was first used in urology, is often used for gynecological caesarean section, is also known as the bikini incision, and because of its concealed incision and good aesthetics it is accepted by the majority of female patients. Today, Pfannenstiel incisions are used by surgeons in laparoscopic surgery for colorectal cancer for specimen extraction [9].
Due to the small number of analyses in the laparoscopy of Pfannenstiel incision in colorectal cancer, this meta-analysis provides a reference for the use of Pfannenstiel incision in laparoscopy of colorectal cancer in order to evaluate the safety of the Pfannenstiel incision in laparoscopy of colorectal cancer to explore surgical incisions that can improve surgical outcomes as well as postoperative prognosis in patients with colorectal cancer.
Material and methods
Search strategy
To comprehensively search for relevant studies published up to March 10, 2023, we conducted a systematic literature review using the following databases: PubMed, Embase, Web of Science, Cochrane Library, CNKI (China National Knowledge Infrastructure), VIP (Chinese Scientific Journals Database), and WanFangData. The search terms used were “Colorectal Cancer” and “Pfannenstiel”, combined with the conjunctions “and” or “or”. The language was limited to English and Chinese. References in selected articles and some potentially relevant articles were also checked to determine the comprehensiveness of relevant studies by hand. The retrieved articles were carefully selected to avoid duplication of data. This study was approved by the Institutional Ethics Committee and Institutional Review Board of Liaoning Cancer Hospital.
Inclusion and exclusion criteria
This study was searched from public databases, so there were no informed consent or ethical concerns. i) The included studies were either prospective or retrospective. ii) A clear statement in the “Material and methods” section. iii) The published literature has studied colorectal cancer patients undergoing laparoscopic surgery. iv) In each paper, the methods of specimen extraction were Pfannenstiel incisions vs. non-Pfannenstiel; v) the related data could be reported and extracted directly or calculated indirectly from the original studies. Case reports, reviews, conference abstracts, and fundamental research studies were excluded.
Data extraction and quality assessment
Three researchers independently selected the trials and extracted the data according to the above-mentioned criteria. The patients who underwent surgery were divided into the Pfannenstiel group and the no Pfannenstiel group according to the location where the specimen was removed during the operation and the following data were collected: the basic data of these articles are author, study period, region, study design, number of patients, age, male, body mass index (BMI), data related to the safety of the Pfannenstiel incision including surgical outcomes: operative time, length of extraction skin incision, and complications: superficial wound infection, incisional hernia, organ/space surgical site infection, complications.
The quality of the data was assessed by two researchers using the Newcastle-Ottawa Quality Assessment Scale (NOS). Studies with ≥ 7 points were regarded as “high quality ”, studies with 4 to 6 points were regarded as “moderate quality ” and studies with ≤ 3 points were regarded as “low quality”. The assessment was done in duplicate, and disagreements were handled by discussion to reach a consensus.
Statistical analysis
Review Manager, version 5.4 (Nordic Cochrane Centre, Copenhagen, Denmark) software and STATA12.0 were used for statistical analysis. In this meta-analysis, the inverse variance method was used for continuous variables and the Mantel-Haenszel method for categorical variables. Heterogeneity was assessed using the I² method: when I² > 50%, there was greater heterogeneity, and a random-effects model was used; when I² ≤ 50%, a fixed-effect model was used. Subgroup analysis was not required for the study. Sensitivity was analyzed by excluding studies on a case-by-case basis for each indicator, and sensitivity was analyzed for pooled results and overall fit. Publication bias was assessed by funnel plots and Begg’s and Egger’s test. In all statistics, p < 0.05 was considered to be significant.
Results
Study characteristics
Our study found 147 documents in total, including 7 documents in the Cochrane Library, 33 in PubMed, 59 in Embase, 21 in Web of Science, 13 in CNKI, 3 in WanFangData, and 3 in VIP; in addition, eight documents were searched by manual and reference searches. After checking the duplicates, 120 documents were left, and then, after reading titles and abstracts, 96 documents were excluded because they were irrelevant. Consequently, a total of 24 documents remained after the initial screening process. Subsequently, these 24 documents underwent a comprehensive full-text assessment, resulting in the exclusion of 19 studies. Among these exclusions, inappropriate populations accounted for 9 studies, inadequate outcomes were observed in 5 studies, and 4 studies lacked relevance to the topic under investigation. Ultimately, only 5 studies met the inclusion criteria and were included in this meta-analysis [4, 5, 8, 10, 11] (Figure 1).
In study characteristics, the total study period was from 2002 at the earliest to 2017 at the latest; as for region, two of the documents were from USA, two from China, and the other two from Turkey and Denmark (Table I). In these documents, four were retrospective experiments and two were prospective experiments. A total of 681 patients were included in the study, including 239 in the Pfannenstiel group and 442 in the no Pfannenstiel group (Table I). In documents of S.T. Orcutt, Feza Y. Karalayali, and Maria Widmar, the median range of patients’ ages was 61–68 years and the median range of percentage of male patients was 52.1–98.2%. The median range of patients’ BMI was 24–28.7 kg/m2 in documents of S.T. Orcutt, Feza Y. Karalayali (Table I). For each incision type included in the study, Xujinghong’s, Orcutt’s, and Maria Widmar’s studies compared midline incisions with Pfannenstiel incisions, and Xujinghong’s study also included lower quadrant oblique incisions, left lower quadrant transrectal incisions, old incisions were compared with Pfannenstiel, Feza Y. Karalayali’s study compared ileostomy site incision with Pfannenstiel incision, M.C. Rasmussen compared supraumbilical transverse muscle-sparing incision with Pfannenstiel incision. As regards the quality of the data, three documents were high quality (NOS ≥ 7), and the other two documents were moderate quality (4 < NOS < 6) (Table I). For sensitivity, we excluded articles from the included studies on an article-by-article basis, and the results of the exclusions matched the overall results.
Table I
Main characteristics of included studies
[i] P – Pfannenstiel group, no-P – no Pfannenstiel group, BMI – body mass index, „/” – Data not available, n – number, NOS – Newcastle-Ottawa Quality Assessment Scale, UAMI – upper abdominal midline incisions, LAMI – lower abdominal midline incisions, LQOI – lower quadrant oblique incisions, LLQTI – left lower quadrant transrectal incisions, OI – old incisions, MI – midline incisions, ISI – ileostomy site incisions, VMI – vertical midline incisions, STMI – supraumbilical transverse muscle-sparing incisions.
Surgical outcomes
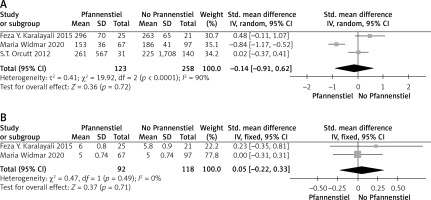
The results of surgical outcome in this study were divided into two parts: one was the operative time and the other was length of extraction skin incision. Our findings showed that there was no significant difference between the two groups in terms of operative time (SMD = –0.14; 95% CI = –0.91 to 0.62; p = 0.72), and there may be a tendency to reduce the duration of surgery in the Pfannenstiel group. In terms of length of extraction skin incision, there was also no significant difference between the two groups (SMD = 0.05; 95% CI = –0.22 to 0.33; p = 0.71), but a tendency to reduce the length of extraction skin incision was observed in the no Pfannenstiel group (Figure 2).
Complications
In our meta-analysis, there were overall complications, superficial wound infection, organ/space surgical site infection and incisional hernia were counted. For overall complications, the results indicated that there was no clear difference between the two groups (RR = 0.76; 95% CI = 0.27 to 2.14; p = 0.60). For superficial wound infection, the results indicated that there was no clear difference between the two groups in superficial wound infection (RR = 1.05; 95% CI = 0.26 to 4.18; p = 0.95). For organ/space surgical site infection, the results indicated that there was no significant difference between the two groups (RR = 0.41; 95% CI = 0.09 to 1.79; p = 0.24), although Pfannenstiel had the potential to decrease the incidence of organ/space surgical site infection. For incisional hernia, Pfannenstiel may reduce the incidence of incisional hernia (RR = 0.48; 95% CI = 0.27 to 0.87; p = 0.01) (Figure 3).
Figure 3
Meta-analysis results for studies comparing Pfannenstiel group vs. no Pfannenstiel group for overall complications (A) including superficial wound infection (B), organ/space surgical site infection (C) and incisional hernia (D)

There was no publication bias in the three studies of operative time, superficial wound infection, and incisional hernia, based on funnel plots and statistical significance (Egger’s p = 0.542, 0.944, 0.997, respectively). For the other three studies (extraction length, skin incision, overall complications, organ/interstitial surgical site infection), there was no evidence of publication bias (Begg’s p = 1.000) (Figure 4).
Discussion
With the first description of laparoscopic right colectomy by Jacobs et al. in the 1990s, the development of minimally invasive surgery for the treatment of colorectal cancer went from hand-assisted laparoscopic surgery (HALS), laparoscopically assisted techniques, totally intracorporeal laparoscopic surgery (TILS) to single-incision laparoscopic surgery (SILS), flexible laparoscopy (FLS), and robotically assisted laparoscopic surgery (RALS) [12, 13]. Several advantages such as the small incisions, the low incidence of incisional hernia and the short hospital stay over traditional open surgery are emerging in laparoscopic colectomy surgery [14–16]. In addition to the advantages in short-term complications, a long-term efficacy advantage has been shown in the treatment of colorectal cancer. It is worth mentioning that in terms of the psychological impact of surgery on patients, Pfannenstiel can reduce the rejection of surgical scars and improve the prognosis of surgery due to its hidden scar location, so laparoscopy colectomy surgery is now the standard technique for colorectal cancer in many countries around the world [17–19]. Especially in terms of safety, compared with traditional open surgery, minimally invasive surgery surely shows comparable or superior outcomes with fewer complications in general [20]. The extraction of a surgical specimen played a vital role in minimally invasive colorectal surgery and the size of the extraction site was limited to the surgical method and the volume of the specimen [21]. However, some studies have indicated that some potential postoperative morbidity including hernia and incision infection resulted from the selection of specimen extraction sites [22]. Even though many specimen extraction methods such as middle incision, transverse, paramedian and natural orifice specimen extraction (NOSE) have been used in laparoscopic minimally invasive surgery for colorectal cancer, the middle incision is still the most commonly used extraction site incision [15, 22]. The Pfannenstiel incision, commonly used in gynecological and urological surgery, is reportedly associated with a lower incidence of wound complications [4, 23]. Due to providing excellent exposure to the rectosigmoid colon, the Pfannenstiel incision is a popular choice for left-sided colon resections [15, 24]. The purpose of this study was to evaluate the feasibility of using the Pfannenstiel incision in minimally invasive surgery for colon cancer.
Our metaanalysis results suggested that the Pfannenstiel incision may have an advantage versus the no Pfannenstiel incision in terms of reducing the duration of surgery and increasing the length of the extraction skin incision. In the evaluation of overall complications, no significant difference was observed between the two groups, but the Pfannenstiel group had the potential to decrease the incidence of overall complications and surgical site infection. It is worth noting that in the incisional hernia evaluation, those patients who underwent Pfannenstiel incision for specimen extraction had a significant reduction in the incidence of incisional hernia. It follows that the Pfannenstiel incision may be a good choice as a specimen extraction incision for laparoscopic surgery in colorectal cancer.
Regarding surgical indicators, we evaluated two indicators: surgical time and incision length. The conclusion was that there was no difference between the Pfannenstiel group and the no Pfannenstiel group in these two indicators, but Pfannenstiel may be associated with shorter surgical time and longer incision length. A study by Takagi et al. mentioned that the length of the Pfannenstiel incision is fixed at 6–-7 cm, and the documents included in our study also reported a similar incision length which was compared to the 5 cm transumbilical incision and seems to be longer, but there is no statistically significant difference [25]. The Pfannenstiel incision requires layer-by-layer suturing, and both transverse and vertical opening methods are used, which increases surgical complexity and surgical time; however, the possible reason for the shorter operation time is that the larger Pfannenstiel incisions are easier to close than other smaller incisions, thus shortening the operation time [25].
Probably due to its anatomy, the complication rate associated with the Pfannenstiel incision was low [4]. Our results also confirmed and indicated that the Pfannenstiel group had the potential to decrease the incidence of complications compared to the no Pfannenstiel group. There is now research showing that the Pfannenstiel incision can reduce the risk of fascial dehiscence and postoperative adhesions, as it is parallel to the tension line of the abdomen and is located at the lowest and least tense point of the abdominal wall [26, 27]. In gynecological surgery, the Pfannenstiel incision has also been shown to be associated with a reduced incidence of postoperative ileus, infection rates, and incisional hernia due to its more limited abdominal exposure [23]. However, the Pfannenstiel incision has been found to be associated with a high rate of nerve entrapment [28]. Currently, the advantages of Pfannenstiel complications still need further exploration.
Surgical site infection (SSI) is the most common nosocomial infection in surgery, and in our study, there was no significant difference in wound infection rates between Pfannenstiel incision and no Pfannenstiel incision [29]. Inaba et al. compared the incidence of wound infection between Pfannenstiel and midline incisions in open surgery, and concluded that there was no difference in terms of wound infection rates [30, 31]. Although our results are consistent with their conclusions, our results have a bias towards the Pfannenstiel incision. In particular, Orcutt’s study showed that the incidence of wound infection with midline incisions was about five times higher than with Pfannenstiel incisions [4]. A retrospective analysis from McCurdy compared the incidence of wound infection with vertical and Pfannenstiel incisions in obese patients undergoing cesarean section, and found a significant advantage in Pfannenstiel incisions [32]. Currently, the advantage of Pfannenstiel incision in terms of wound infection rate is unclear, and further studies are needed to probe in this area. As for organ/space surgical site infections, the results were similar to SSI. This result can be explained by the observation that compared to the midline incision, the lower incidence trend of incision infection in Pfannenstiel incision may be due to the anatomical characteristics of the transverse incision of Pfannenstiel, which helped preserve the fibrous sheath in front of the rectus abdominis muscle, an important fibrous sheath used to maintain stability in the lower abdomen. The damaged muscle in this incision was covered by healthy uncut tissue, and there was lower incidence of complications such as wound infection, while the cutting of all layers of the midline incision was in the same plane, and the risk of complications such as wound infection, hematoma and so on was increased [24]. In general, Pfannenstiel incision has no clear differences versus no-Pfannenstiel incision in reducing infection rates.
For the study of incisional hernia, Benlice et al. found that the choice of location for specimen extraction in colorectal laparoscopic surgery is the most critical and modifiable variable affecting the incidence of incisional hernia; simultaneously, their research also showed that the incidence of Pfannenstiel’s incisional hernia was 13 and 28 times lower than midline incisions and stoma sites, respectively [33]. The most significant finding in DeSouza’s study was that hand-assisted laparoscopic surgery with a Pfannenstiel incision had a lower incidence of incisional hernias compared to open surgery and midline incisions, and even reached 0% incisional hernia incidence [23]. A meta-analysis in 2017 also noted that the incidence of incisional hernia in midline incisions for specimen extraction in laparoscopic surgery was four times higher than non-midline incisions, and significantly lower when compared to Pfannenstiel incisions [34]. Our study’s results were consistent with the conclusions of the above-mentioned studies. Regarding the reasons for this result, on the one hand, due to the way the Pfannenstiel incision is cut in the direction of the muscle fibers, the blood supply to the muscle bed is preserved and the wound heals easily; on the other hand, when the internal pressure increases, the incision on the rectus abdominis sheath forms an angle to the rectus abdominis muscle, and incision hernia is less likely to occur [23, 33]. It is worth noting that a special cutting method, which involves making a horizontal incision in the direction of the skin and subcutaneous tissue and rectus sheath, followed by a vertical incision in the muscle and peritoneum, can also be a reason for the lower incidence of incision hernia with the Pfannenstiel incision [25].
Our study still had many limitations. The main limitations were that the included documents were few and concerned few cases, ultimately subgroup analyses could not be performed, and most of the included studies were retrospective, resulting in high levels of bias. Moreover, there is no consensus on the best tool to assess the quality of non-randomized randomized studies, and NOS is used by us, but there are other methods of evaluation.
Conclusions
In colorectal cancer patients, the Pfannenstiel incision used for laparoscopic surgical specimen extraction is associated with a significant reduction in the incidence of incisional hernia over no Pfannenstiel. The patients undergoing the Pfannenstiel specimen extraction had a potential low incidence of overall complications and surgical site infection. Although the relevant research is not sufficient, we believe that the Pfannenstiel incision is still a good incision for the extraction of laparoscopic surgical specimens in colorectal cancer patients, and we hope that our study will inform clinical work.