A 65-year-old man presented to the emergency department with a transient anterior-wall ST-elevation myocardial infarction (STEMI) (Figures 1 A, B). The patient had a history of percutaneous coronary intervention (PCI) to proximal left anterior descending artery (LAD) 3 months prior this acute admission. Dual antiplatelet therapy was erroneously interrupted for 7 days in the context of an elective dental procedure.
Figure 1
A – Electrocardiogram (ECG) taken in the Emergency Department at the onset of chest pain with anterior STEMI. B – ECG repeated 30 min after the first ECG, when chest pain had completely resolved, showing complete ST-segment resolution before cardiac catheterization. C – Index coronary angiogram with appearance of proximal left anterior descending (LAD) stent thrombosis (white arrow). D – Repeat angiogram after 5 days of intensive antithrombotic therapy, showing patent LAD stent with complete resolution of thrombus. D 1, 2 – Optical coherence tomography confirmed adequate expansion of the stent throughout its full length, complete apposition of the struts to the vessel wall and lack of edge dissection
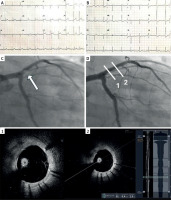
The patient was loaded with aspirin and ticagrelor and even though emergency coronary angiogram showed stent thrombosis in the proximal LAD, there was thrombolysis in myocardial infarction (TIMI) 3 flow (Figure 1 C). Due to the high thrombus burden and relief of symptoms, procedure was deferred, and the patient was put on intravenous (IV) tirofiban infusion for 18 h along with subcutaneous low molecular weight heparin (LMWH) therapeutic dose and dual antiplatelet therapy (DAPT) with aspirin and ticagrelor. The repeat angiogram after 5 days showed a patent LAD stent with complete resolution of the thrombus (Figure 1 D). Optical coherence tomography (OCT) using the Gentuity HF-OCT Imaging System with the Vis-Rx Micro-Imaging Catheter (Nipro Medical Europe, Nipro European HQ, Blokhuisstraat 42, 2800, Mechelen, Belgium) confirmed the adequate expansion of the previously implanted stent in its full length, complete apposition of the stent struts to the vessel wall and lack of edge dissection (Figure 1 D 1, 2). It was therefore decided to administer conservative treatment. Peak hs-cTn was 70 ng/l and BNP level 310 pg/ml. The patient was symptom-free at 3 months follow-up.
Up to 1 out of 4 patients who initially present with a STEMI may subsequently show complete resolution of symptoms and ST elevation before revascularization therapy is initiated [1]. This condition is called ‘transient STEMI’. Augmented endogenous fibrinolysis has been found in such patients, who appear to have a more favorable prognosis with smaller infarct size compared to patients with persistent STEMI [1]. According to the PLATO trial, rapid clot lysis is a strong independent predictor of favorable outcome in STEMI patients, independent of their antiplatelet therapy [2]. Fibrinolysis is not mediated by oral antiplatelet medication. Therefore, an intense parenteral antithrombotic therapy is warranted, as in our patient.
In our institution, in cases of high thrombus burden and a deferred procedure, we administer an IV GP IIb/IIIa inhibitor for 18 h after the diagnostic procedure on top of DAPT and a therapeutic dose of LMWH and then, following interruption of the GP IIb/IIIa inhibitor, triple antithrombotic therapy for 5–7 days. The usual time elapsed is 24–72 h in the randomized controlled trials (RCT) except INNOVATION, which used a time lag of 3–7 days. Similarly, the majority of the 10 non-RCT studies also used a time delay between 24 and 72 h [3]. Only four studies have used a longer, 6–7-day window period for deferral [3]. Many researchers, including our group, consider the 24–48-hour window period too short for thrombus resorption and effective action of antithrombotic agents.








