Purpose
For patients with high-intermediate risk (HIR) endometrial cancer, adjuvant radiation therapy (RT) reduces the risk of recurrence [1, 2]. The PORTEC-2 study demonstrated that vaginal cuff brachytherapy (BT) was as effective as pelvic external beam radiation therapy (EBRT) in preventing vaginal recurrence (1.6% vs. 1.8%, p = 0.7) [3]. Patients treated with EBRT had a lower rate of pelvic recurrence (0.5% vs. 3.8%, p = 0.02), but the absolute rate of pelvic recurrence remained low in the vaginal BT arm [3]. Given a favorable side effect profile and patient convenience, vaginal cuff BT is generally preferred in HIR cases, particularly in patients who have undergone comprehensive nodal assessment [4]. In addition to the local recurrence benefit demonstrated in randomized clinical trials, National Cancer Database (NCDB) analyses have found an overall survival benefit of adjuvant RT compared with surgery alone in HIR patients [5-7]. The executive summary of ASTRO guidelines recommends adjuvant BT over observation for grade 1 or 2 endometrial cancers patients with ≥ 50% myometrial invasion (MI) (stage IB) or grade 3 tumors with < 50% MI (stage IA) [4]. However, a substantial proportion of these patients do not receive guideline-recommended adjuvant RT. A report by Zakem et al. showed that observation was the most common approach for HIR endometrial cancer patients in the NCDB, with 58.1% of patients observed in 2010 [8].
The Patient Protection and Affordable Care Act (ACA) was signed in 2010 with the aim of improving access to healthcare through expanding insurance options, including the expansion of Medicaid [9]. A 2012 Supreme Court ruling gave the option for states to implement certain new health insurance requirements and ultimately, most Medicaid expansion went into effect in January 2014 [10]. States that expanded Medicaid in January 2014 according to NCDB coding were Kentucky, Nevada, Colorado, Oregon, New Mexico, West Virginia, Arkansas, Rhode Island, Arizona, Maryland, Massachusetts, North Dakota, Ohio, Iowa, Illinois, Vermont, Hawaii, New York, and Delaware. States that expanded in 2010-2013 were Washington, California, New Jersey, Minnesota, and Connecticut in addition to the District of Columbia. The decision of the remaining states not to expand Medicaid left many patients without an affordable insurance coverage option, which could lead to barriers to accessing healthcare, resulting in delayed disease detection and treatment. Previous research by Han et al. demonstrated that disparities in the percentage of uninsured patients by race, income level, and rurality were decreased or eliminated in states that expanded Medicaid with the ACA, but remained high in states that did not expand Medicaid [11]. The effect of Medicaid expansion on the receipt of guideline-indicated adjuvant RT in endometrial cancer patients in general has not been previously reported.
Therefore, the goal of the present study was to determine the effect of Medicaid expansion, and subsequent decrease in uninsured patients, on the receipt of RT after surgery in endometrial cancer patients. The hypothesis was that lack of insurance might be driving underutilization of endometrial cancer patients to undergo adjuvant RT (stage IA and grade 3, or stage IB and grade 1 or 2), who would be more likely to receive indicated adjuvant RT if they resided in states that expanded Medicaid compared with patients in states that did not expand Medicaid.
Material and methods
The NCDB was used to identify patients with endometrial adenocarcinoma, stage IA and grade 3 or stage IB and grade one or two, diagnosed from 2010-2018. The NCDB is a cancer outcomes database derived from hospital registry data, which captures approx. 70% of patients with newly diagnosed cancer in the United States. Medicaid expansion data is suppressed in the NCDB for patients < 40 years old, and patients ≥ 65 years old are generally eligible for Medicare; thus, patients aged 40-64 were included in the current study.
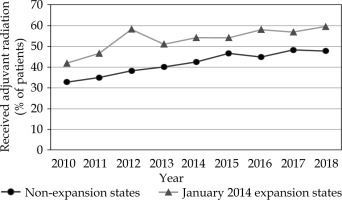
We used a standard statistical approach for evaluating the influence of a health policy change in a quasi-experimental fashion [12]. A difference-in-differences (DID) cross-sectional retrospective analysis using a multivariable linear regression was conducted, comparing the change in the percentage of patients who received guideline-indicated adjuvant RT among patients residing in Medicaid expansion and non-expansion states, diagnosed before and after ACA implementation. Parallel trends in pre-exposure time period were verified visually (Figure 1) and by regressing a year-expansion interaction term on the receipt of adjuvant RT in pre-expansion period (interaction non-significant). Variables that were significantly different between expansion and non-expansion states on univariate analysis (Table 1), and those known to be important for disease outcomes in endometrial cancer were included in the final multivariable model. Included variables were age, race, insurance status, income quartile, rurality, Charlson-Deyo comorbidity score, lymphovascular space invasion (LVSI), and receipt of regional nodal surgery when applicable.
Table 1
Descriptive statistics by expansion group
Given that 24 states and the District of Columbia expanded their Medicaid programs on or before January 1, 2014, this date marked the beginning of post-expansion period in our main analysis, which included data from January 1, 2010, to December 31, 2018. Patients who received EBRT were grouped with patients who received BT for the initial analysis. Sensitivity analysis was performed with EBRT patients grouped with patients who did not receive any adjuvant treatment, with DID analysis comparing the change in the percentage of patients who received adjuvant BT only among patients residing in Medicaid expansion and non-expansion states, diagnosed before and after ACA implementation.
Results
The total number of patients who met entry criteria was 8,847, including 4,197 patients (47.4%) in states that expanded Medicaid on or before January 2014, and 4,650 patients (52.6%) from states that did not expand Medicaid. Distributions of age, race, primary insurance status at diagnosis, income quartile by zip code, rurality, Charlson-Deyo comorbidity score, LVSI, and receipt of regional nodal surgery were similar in expansion and non-expansion states (Table 1). Median age was 59 years (range, 40-64 years).
Table 2 provides the proportion of patients who received adjuvant RT in the time before (2010-2013) and after Medicaid expansion (2014-2018), and DID estimates of changes in the percentage of patients who received adjuvant BT. The states that expanded Medicaid had higher rates of adjuvant BT prior to January 2014 than non-expansion states (49.21% vs. 36.46%). After adjustment for socio-demographic factors, Medicaid non-expansion states experienced a 2.68 percentage point (ppt) greater increase in the percentage of patients who received adjuvant RT compared with the expansion states (crude: 9.63 vs. 7.45 ppt; adjusted DID: –2.68 [95% CI: –7.12-1.75]). These findings were not statistically significant (p = 0.236). The proportion of HIR endometrial cancer patients who received adjuvant RT increased over the study period across both Medicaid expansion and non-expansion states (Figure 1). The non-expansion states had a slightly larger absolute increase in adjuvant radiation, resulting in a non-significant change in the difference in adjuvant radiation rates compared with baseline.
Table 2
Changes in the percentage of patients receiving radiation therapy associated with Medicaid expansion among patients aged 40 to 64 years with newly diagnosed cancer
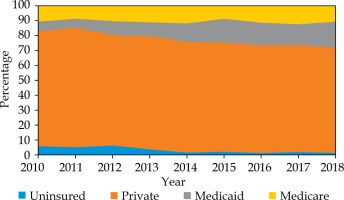
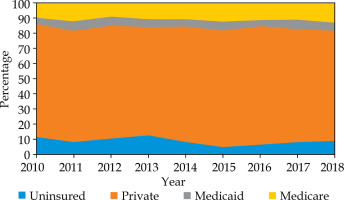
Figures 2 and 3 demonstrate the changes over the study period in primary insurance payor at diagnosis in expansion and non-expansion states, respectively.
The sensitivity analysis compared patients who received adjuvant EBRT with those who did not receive any adjuvant RT, and revealed similar results (supplementary data). Expansion states had higher rates of adjuvant BT prior to January 2014 compared with non-expansion states (36.58% vs. 26.75%), and the proportion of patients who received adjuvant radiation increased over the study period across both Medicaid expansion and non-expansion states. After Medicaid expansion, the expansion states had a larger percentage point increase in adjuvant BT (although non-significant), resulting in a larger difference in adjuvant BT rates (adjusted DID: 0.25 [95% CI: –4.03-4.53], p = 0.909).
Discussion
Our results demonstrate that states, which expanded Medicaid by January 2014 had higher rates of adjuvant RT in HIR endometrial cancer patients at baseline, but expansion of Medicaid and subsequent decrease in proportion of uninsured patients did not significantly increase the proportion of patients who received guideline-concordant adjuvant RT compared with non-expansion states. Therefore, Medicaid expansion and subsequent access to health insurance is likely not the most significant factor affecting access or receipt of adjuvant RT over the study period.
State Medicaid expansions to low-income adults has been associated with an improved coverage, access to care, and health outcomes [13]. Studies have demonstrated improvements in insurance coverage for endometrial cancer patients after implementation of the ACA [14-16]. Moss et al. found that the ACA resulted in an expanded insurance coverage for women diagnosed with a gynecologic cancer, with uninsured rates decreasing by half (6% to 3% for uterine cancer), when comparing the 2011-2013 sub-group with those diagnosed in 2014 in states with expanded Medicaid eligibilities [14]. Jemal et al. showed that the percentage of uninsured patients with newly diagnosed cancer declined substantially after the ACA, especially among low-income patients in Medicaid expansion states [15]. Another study by Chino et al. analyzed patients in the Surveillance, Epidemiology, and End Results (SEER) registry who received radiation as part of cancer treatment, and found uninsured rates dropped in all states for the year 2014 compared with 2010-2013, but the magnitude was larger in Medicaid expansion states [17]. A research by Spiegel et al. that studied patients with gynecologic cancers (including endometrial) treated with BT from SEER showed that states, which expanded Medicaid had a significant reduction in the proportion of uninsured patients from 2.9% to 1.8%, p = 0.026, while non-expanded states had a non-significant increase in the proportion of uninsured patients. For patients with uterine cancer, there was a decrease from 3.4% to 1.6% in uninsured rates in expanded states, p = 0.006 [18]. In contrast to the nationwide NCDB used in our study, the SEER database includes population-based cancer registries in 14 states. Overall, these studies provide evidence that the ACA led to an increased insurance rates for endometrial cancer patients, with a suggestion that there was a greater effect in Medicaid expansion states.
Increases in insurance coverage may help to achieve improvements in access to cancer care and better quality, but changes to and from private insurance may make it more difficult to assess the impact of Medicaid. Fader et al. reported that for endometrial cancer patients in the NCDB, stage I endometrial cancer patients with Medicaid were more than twice as likely to die after primary surgical treatment compared with patients covered with private insurance (HR = 2.34 for overall survival [OS]). Rates of adjuvant radiation were not reported for early-stage disease in this study [19]. Barrington et al. performed an NCDB study comparing uninsured rates in endometrial cancer patients before and after the ACA, and found a decline in the proportion of uninsured patients in both expansion and non-expansion states, with a corresponding increase in private insurance coverage among patients in non-expansion states. Overall, the DID analysis found that Medicaid expansion was associated with an increase in the percentage of endometrial cancer cases who were insured, with 1.4% (95% CI: 0.9-2.0, p < 0.0001) [16]. Agarwal et al. analyzed cancer patients from the SEER database diagnosed between 2011 and 2015, and found that in expansion states, there was a shift in insurance to Medicaid from non-Medicaid insurance (including private insurance, Medicare, and military insurance), while in non-expansion states, an increase in non-Medicaid insurance was noted [20]. In our study, Figure 2 shows a trend towards a decrease in uninsured patients with HIR endometrial cancer in expansion states and a corresponding trend towards an increase in patients with HIR endometrial cancer with Medicaid. This trend is not evident among patients in non-expansion states (Figure 3), but instead, there appears to have been a decrease in uninsured patients with HIR endometrial cancer in 2015 and an increase in patients with HIR endometrial cancer with private insurance. Therefore, changes in rate of private insurance with the ACA may have also contributed to changes in rates of patients receiving adjuvant radiation and overall outcomes.
Other contributing factors to disparities in receipt of adjuvant treatment could be socio-economic status, race/ethnicity, education level, comorbid conditions, distance to treatment center, type of treatment center (comprehensive cancer center vs. not comprehensive), and geographic location. After the ACA implementation, a decrease in inequalities in access to care associated with race was reported by Hayes et al. among the general population across the United States, suggesting that marketplace exchanges may have led to limiting disparities [21]. In contrast, a study of patients with cancer by Han et al. observed a decrease in disparities found only in states that expanded Medicaid, suggesting that the effect of marketplace exchanges may be more of a minimal effect among cancer patients who have higher baseline insurance rates [11]. The scarcity and centralized nature of radiation facilities, and the even greater scarcity of facilities that offer BT, are likely to exacerbate the effects of demographic factors on disparities in access and utilization of adjuvant treatment.
Limitations of the analysis include that the insurance variable only provides information about the insurance status at time of diagnosis, and there is no information reported about changes in insurance status following diagnosis. Patients with cancer may gain Medicaid insurance coverage at time of diagnosis of cancer, and then lose eligibility for insurance coverage after completion and not have proper follow-up. However, this limitation would not significantly impact the results, given it could occur in both expansion and non-expansion states. Additional limitations are that the NCDB reports’ income quartile by zip code is a proxy for patient income, and differences have been shown to be largest among low-income patients [15]. Focusing on the Medicaid expansion part of the ACA may not provide a full understanding of the changes in insurance affecting outcomes.
Conclusions
Medicaid expansion is likely not the most significant factor affecting access or receipt of adjuvant RT in HIR endometrial cancer patients. Further study could help lead to improved understanding of the barriers to healthcare access, inform policy, and efforts to ensure that all patients have access to RT.