Purpose
Utilization of brachytherapy for the management of localized prostate cancer is decreasing in the United States [1]. Studies using large cancer registries have explored these trends, including a study by Martin et al. using the National Cancer Database (NCDB) that identified a change in utilization from 17% in 2002 to 8% in 2010 [2], and a study by Mahmood et al. using the Surveillance, Epidemiology, and End Results (SEER) Program Registry that identified a decrease in brachytherapy procedures from 44% in 2004 to 38% in 2009 [3]. A more recent review of the SEER registry data demonstrated that the use of both monotherapy and combination brachytherapy in prostate cancer decreased by more than 60% from 2004 to 2013 [4]. This decrease in utilization contrasts with high quality data demonstrating the efficacy and favorable quality of life outcomes for patients treated with brachytherapy monotherapy, or as part of combined modality therapy with external beam radiation for high risk disease where significant biochemical progression-free-survival (bPFS) improvements have been demonstrated [5,6,7]. In light of the operator dependency of brachytherapy, however, cautionary data on increased toxicity of brachytherapy given as a boost to external beam radiation therapy (EBRT) or when sub-optimally applied [8,9,10,11] have increased the focus on establishing high quality implant technique, and therefore training of radiation oncology residents.
The decreased utilization of prostate brachytherapy has reduced exposure to the procedure during residency training. For instance, Compton et al. reported a significant decline in per resident logged prostate interstitial brachytherapy cases between academic years (AY) 2006-2007 (2440 procedures total, 114 residents, 21.4 procedures/resident) and AY 2010-2011 (2326 procedures total, 129 residents, 18 procedures/resident) [12]. Continuing this trend, a survey of U.S. chief residents between 2013 and 2015 demonstrated very high rates of respondents noting no or an inadequate level of exposure (40-85%) to prostate brachytherapy procedures (low dose rate – LDR, or high dose rate – HDR) [13].
The “see one, do one, teach one” principle of procedure education that dates back to Halsted is one of the foundations of surgical and interventional procedure training, but without adequate exposure to a critical supply of cases, residents will not be comfortable with the procedure and will be less likely to perform it as a practitioner. The quality of brachytherapy implantation is also likely to be impacted even for those engaged in the practice of brachytherapy, as low procedural volume has also been shown to impact outcomes [14]. Currently, the Accreditation Council for Graduate Medical Education (ACGME) requires a minimum of five interstitial brachytherapy cases (all disease sites combined) to graduate Radiation Oncology residency; however, this minimum requirement is likely insufficient, as many practicing physicians do not feel comfortable enough with their proficiency in the procedure to establish their own brachytherapy practice, and the interstitial case requirement may be satisfied without even performing a single prostate brachytherapy case. Furthermore, given the decreased utilization of brachytherapy described above, access to cases is limited and residents may need to find other ways to increase their exposure to procedural skills necessary to perform brachytherapy treatment.
In the report by Compton et al., it was recommended that the community interested in training residents in brachytherapy should “consider methods to ensure that residents obtain sufficient experience in the future” [12]. Prostate brachytherapy is a complex, multi-step procedure that requires expertise in multiple underlying technical skills, or ‘competencies’, to perform safely and effectively. Gallagher et al. discussed the concept of skill acquisition through skills generalization and skill transfer [15], and it may be possible to develop competencies necessary for prostate brachytherapy by performing other procedures used in the radiation oncology clinic. Transperineal rectal spacer placement (TRSP) is one such procedure, where a material is injected transperineally under ultrasound guidance into the potential space between the rectum and prostate prior to radiation therapy for prostate cancer to increase separation between the structures and reduce incidental radiation dose delivery to the rectum [16]. There is substantial overlap in the generalizable skills or competencies between prostate brachytherapy and TRSP procedure domains, such as patient positioning, transrectal ultrasound imaging, needle placement, and complications management. Thus, mastering fundamental competencies in the TRSP domains may benefit performance of prostate brachytherapy.
In order to better characterize trainee competence, prior studies in internal medicine have used resident “comfort level” (ranging from 1 – very uncomfortable to 5 – very comfortable performing the procedure) in conjunction with minimum requirements established by the ACGME [17]. To better clarify competence for specific types of interstitial brachytherapy, trainee comfort could be used to assess critical procedural skills. This work describes the assessment of teaching techniques focusing on performance of key procedure competencies that are shared with interstitial prostate brachytherapy (PB) and transperineal rectal spacer placement (TRSP).
Material and methods
For PB and TRSP, key competencies were identified; 8 for PB and 7 for TRSP (Table 1). Four of these procedures (patient positioning, transrectal ultrasound imaging, needle placement, and complications management) are shared between PB and TRSP. Fiducial placement is a needle placement procedure that may actually be identically performed in both PB and TRSP; placement of needles for hydrodissection and spacer placement in TRSP is felt to be analogous to needle placement in PB as well.
Table 1
Core competencies for transperineal rectal spacer placement (TRSP) and prostate brachytherapy (PB)
The placement of TRSP has been described previously [18]. At our institution, we use an FDA-approved polyethylene glycol hydrogel (SpaceOAR; Augmenix, Inc., Bedford, MA USA; now Boston Scientific, Inc.). Briefly, the procedure takes place either in a clinic setting with local anesthesia/moderate sedation or in the operating room under general anesthesia per patient preference or if clinic placement cannot be tolerated. Prior to the procedure, the patient is instructed to perform an enema. During the procedure, the patient is placed in the dorsal lithotomy position and the transrectal ultrasound (TRUS) is placed with a stepper for visualization. In the clinic setting, local anesthesia is used in the subcutaneous perineal area and bilateral neurovascular bundles, and moderate sedation with intravenous midazolam and fentanyl is provided; in the operating room setting, the patient is placed under general anesthesia and no local anesthesia is used. Gold fiducial seed markers are then placed with a transperineal approach. An 18 gauge needle is then inserted with the transperineal approach and guided to Denonvilliers’ fascia where hydrodissection takes place. Once adequate separation between the rectum and prostate is visualized on ultrasound, the injectable spacer gel is introduced (Figure 1).
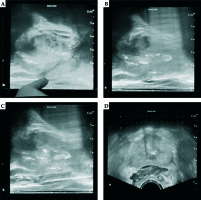
Fig. 1
Transperineal spacer placement; A) identification of rectoprostatic space on transrectal ultrasound; B) needle placement and hydro-dissection; C) rectal spacer insertion; D) rectal spacer material in place between prostate and rectum (axial view)
Prior to involvement in TRSP procedures, the attending reviews the competency steps involved and relevant ultrasound anatomy. Use of prostate phantoms (CIRS Model 053S Tissue Equivalent Prostate Phantom; Computerized Imaging Reference Systems, Incorporated, Norfolk, VA USA) provided initial exposure to ultrasound setup, imaging, and needle visualization and placement (Figure 2) following the method of Thaker et al. [19]. For the first patient, the attending demonstrates the procedure in full with the resident observing; subsequent procedures incorporate direct resident involvement.
Trainee involvement in TRSP has been implemented at our institution for approximately 12 months, and “comfort level” with these procedures (as measured on a Likert scale, Table 2) was assessed prior to and following participation in these procedures. “Comfort level” was graded on a scale of 0-3, with 0 corresponding to the resident having no comfort at all with the procedure, to 3 corresponding to the resident being comfortable with performing the procedure completely independently. Trainees were also asked how many procedures they felt (in their opinion) they would need to perform to reach independent competency. Statistical comparisons were performed using IBM SPSS Statistics v.25.0 (IBM, New York, NY USA); “comfort level” comparisons were performed using the paired sample t-test.
Results
Over a 12-month period, 8 of 12 trainees at our institution participated in TRSP procedures. Two of these trainees had prior experience with prostate brachytherapy or other endorectal procedures and were excluded from further analysis. Prior to performing TRSP procedures, median comfort level for competency domains relevant to prostate brachytherapy included: patient positioning (median 1, range 0-2); transrectal ultrasound imaging (median 1, range 0-1); needle placement domains: fiducial placement (median 1, range 0-1); hydrodissection (median 0, range 0-1) (Table 3).
Table 3
“Comfort level” assessment of trainees before and after transperineal rectal spacer placement (TRSP) procedure training
Median number of TRSP procedures performed by assessed trainees during the analysis period was 4 (range 1-6). Following TRSP procedure training, median comfort level increased by 2 points for patient positioning (median 3, range 1-3; p < 0.01) and by 1.5 points for transrectal ultrasound imaging (median 2.5, range 1-3; p < 0.001). Needle placement domains improved by 1 point for fiducial placement (median score 2, range 1-3; p < 0.001) and by 1.5 points for hydrodissection (median score 2, range 1-3; p < 0.001).
No trainees felt that they were ready to perform all competencies for TRSP independently at the end of the evaluation time point, responding that a median of 5 additional cases overall would be necessary for “independent” competency (Table 4). However, 66.7% of residents felt that they were fully independently competent in patient positioning, and 50% felt that they were fully independently competent in ultrasound use and local anesthesia. 33.3% felt that they were fully independently competent in fiducial placement and hydrodissection. Of note, in all cases where the resident stated that they had reached the “independent” comfort level in a competency, their performance in that competency was noted by the observing brachytherapy procedure attending to be satisfactory. As directly observed by brachytherapy procedure attendings during subsequent prostate brachytherapy cases, those residents who had reached the “independent” comfort level for procedure skills in patient positioning and transrectal ultrasound use were able to perform those skills independently for PB procedures. All (100%) of the residents felt that procedure education with TRSP placement had a positive impact on their confidence and competencies with transperineal prostate brachytherapy procedures.
Table 4
Range of self-reported additional cases necessary for trainees to reach “independent” competency in transperineal rectal spacer placement (TRSP) procedures
| TRSP procedure | Range | |
|---|---|---|
| Patient positioning | 1-6 | |
| Transrectal ultrasound imaging | 3-6 | |
| Needle placement domains: | ||
| Fiducial placement | 3-10 | |
| Hydrodissection | 4-10 | |
Discussion
Achieving clinical competency in core procedures relevant to the practice of radiation oncology is a primary concern for residency education. Numerous studies have shown that in prostate brachytherapy, implant quality is critical to achieve optimal outcomes as biochemical progression-free survival is significantly linked to the dose received by 90% of the prostate volume (D90) [20,21], and urinary toxicities are also closely associated with urethral dosimetric quantities [22]. Dosimetric guidelines have been provided by the American Brachytherapy Society (ABS) and the American Association of Physicists in Medicine (AAPM) [23,24,25].
Given the technical nature of seed placement and the importance of implant dosimetry, decreased exposure to prostate brachytherapy during residency is concerning and may deter physicians from offering brachytherapy as a treatment option. Additionally, decreased brachytherapy experience may be dangerous to patients as those treated by higher volume physicians were found to have a lower risk of recurrence and a lower risk of prostate cancer death [6,11]. Furthermore, reporting requirements specified by the Nuclear Regulatory Commission may further dissuade providers from offering brachytherapy as minor underdosing can be classified as a reportable error [1], making brachytherapy a potential liability. Finally, the shift away from brachytherapy to newer and more expensive therapies places a significant financial burden on the healthcare system and patients. In the future, development of alternative payment models may incentivize brachytherapy because of its efficient and cost-effective nature, further emphasizing the importance of prostate brachytherapy experience during residency training. Lastly, with data suggesting meaningful benefits to combination brachytherapy boost, where toxicity is increased, an increased proportion of PB in the future is likely to require a mix of HDR/LDR skill sets and harbor a narrower therapeutic margin in terms of operator competency effect on treatment toxicity.
Thus, high quality procedural education and training is of the utmost importance for patient care and safety, for physician efficacy, and for the economic impact of our increasingly robust medical management of cancer. As the use of brachytherapy declines, it is important to integrate the technical skills involved with the procedure into resident education and to ensure that enough repetitions occur so that the trainees feel comfortable performing certain key competencies. Our observed increase in trainee comfort levels across all categories of assessed TRSP procedure components indicates that simple component training could be an important aspect of all radiation oncology training programs. With mastery of some key components, residents will be able to focus on developing overall higher comfort levels with other aspects of prostate brachytherapy procedures, which in turn could help to counteract downward trends in the use of prostate brachytherapy as trainees gain the confidence to perform the necessary procedures. More importantly, prostate brachytherapy could become an even safer and more effective prostate cancer therapy option as increased physician comfort and subsequent increased experience lead to lower recurrence rates and lower prostate cancer death risk. This is supported by similar work in gynecologic brachytherapy, where proficiency-based training was recently reported by Zhao et al.; they showed that simulation training in the setting of cervical cancer brachytherapy showed improvements in resident performance [26].
There are several limitations of the study, primarily sample size. Only six trainees were studied, but the ease of implementing the training and the simplicity and expediency of the surveys indicate that this evaluation could be replicated on a larger scale or even at a prostate brachytherapy-specific school such as the American Brachytherapy Society Prostate Brachytherapy School. The assessment of comfort level itself is limited; prior studies in internal medicine using resident “comfort level” to assess common procedural skills noted that resident comfort did not necessarily correlate to completion of ACGME requirements (for some procedures, comfort was achieved before meeting requirements, while it was not achieved until far exceeding requirements for others) [17]. Another limitation of the study is that it only assesses comfort levels in specific competency domains shared by PB and TRSP. Evaluating global improvements in the ability to deliver PB is well beyond the scope of this study, and we would recommend implementing this study on a larger scale with more participants and including evaluation of comfort levels during a prostate brachytherapy procedure itself before and after TRSP procedure training. Requiring more repetitions per trainee could also produce more robust results, as trainees indicated that they would need more cases in order to reach “independent” competency (Table 4). The study could also be expanded to include other specialized procedures involving these same TRSP components. This could be easily implemented at any institution with a high-volume radiation oncology center and physicians who are proficient in such procedures.
Conclusions
Optimally, all radiation oncology trainees will be exposed to sufficient prostate brachytherapy volume to be comfortable with all skills relevant to the procedure prior to entering independent practice, but this is currently not the case for many graduates. Increasing trainee involvement in related procedures that allow development of shared core competencies may help facilitate increased comfort with critical procedural skills. Overall, skill acquisition and transfer from TRSP could improve patient care and encourage the utilization of prostate brachytherapy.




